The UK’s National Institute for Health and Care Excellence (Nice) has declined to recommend two new Alzheimer’s drugs for routine NHS use in England. While disappointing for some families affected by dementia, this decision reflects a cautious and evidence-based approach that protects patients and public funds.
The drugs in question – lecanemab, made by Eisai, and donanemab made by Eli Lilly – have received significant attention, with headlines hailing them as “breakthrough” treatments and “miracle” drugs. However, Nice has a long history of closely scrutinising new dementia drugs – and, as in previous cases, it has raised important questions about how much benefits these medicines actually provide.
The main claim is that these drugs can delay the progression of Alzheimer’s by about four to six months in people with early-stage disease. That’s not nothing – but it’s also not the dramatic shift some headlines imply.
It’s also important to distinguish between clinical trial results and how treatments perform in everyday care. Trial conditions are controlled and selective, whereas the NHS treats a much broader mix of patients.
Get your news from actual experts, straight to your inbox. Sign up to our daily newsletter to receive all The Conversation UK’s latest coverage of news and research, from politics and business to the arts and sciences.
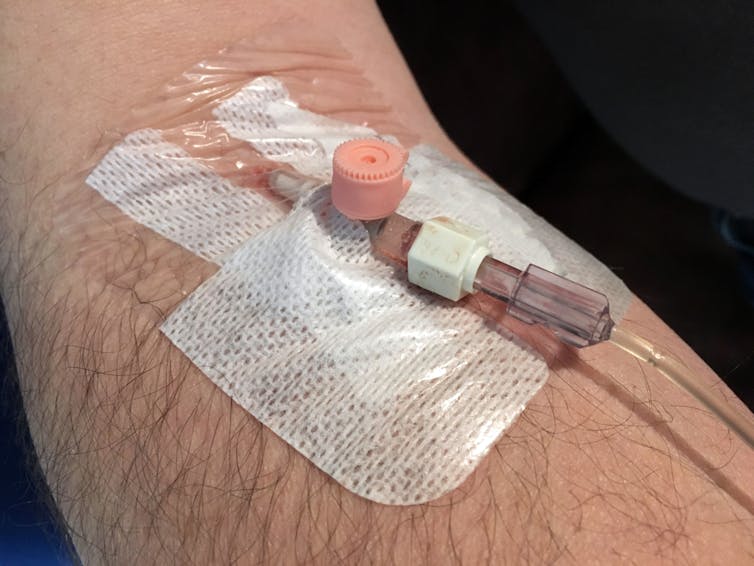
There are other factors to consider, too. These drugs come with risks – including the potential for brain swelling and bleeding – and require invasive testing, such as lumbar puncture or regular brain scans, before and during treatment. The infusions must also be delivered at a hospital infusion over many months. For some patients, that burden may outweigh the modest benefit.
Another issue is that we don’t yet know whether the benefits last beyond the 18-month trial period. Nice must base its decisions on long-term projections, using well established tools such as the quality-adjusted life year to weigh the health benefits against the cost to the NHS. These decisions often involve complex models – and reasonable people may interpret the evidence differently.
Cost plays a role too. In the US, the drugs are priced at up to £25,000 per patient per year. While companies can offer discounts to the NHS, Nice must still consider whether the same money might do more good elsewhere in the health system.
In this case, Nice concluded that the benefits of the new Alzheimer’s treatments are still too small to justify the additional costs at the current price point – a decision supported by some experts.
Tom Dening, professor of dementia research at the University of Nottingham, described the benefits as “minimal” and warned they could distract from other priorities, such as providing good care and support for people already living with dementia.
Heated debate
Nonetheless, the debate has become heated. Some drug companies have argued that the UK system is flawed, suggesting that even offering their drug for free would not be enough to secure approval. But this misunderstands how Nice works. Evaluating the full cost – not just of the drug, but of scans, infusions and monitoring – is not a flaw, it’s part of responsible decision-making.
There are echoes here of earlier disputes from the 2000s when companies tried to publicly pressure Nice to change its decisions. However, history suggests that this strategy rarely works. Ministers have consistently supported Nice’s independence, and the agency’s record shows that it usually says “yes” – or at least yes under certain conditions – even to very expensive drugs, where the evidence supports their use.
The current decision is still technically a “final draft”. Both companies have until July 3 to comment or appeal. In 2007, Eisai took Nice to court – and lost. This time, an appeal is more likely.
Understanding the principles behind Nice’s decision helps put this outcome in context. These are not decisions taken lightly. They reflect a careful balance of evidence, risk, cost and benefit to patients – and, crucially, a commitment to fairness in how NHS resources are used.
Paul Atkinson received funding from the Wellcome Trust for the research on which this article draws.
Sally Sheard has received funding from Wellcome, NIHR, UKRI and the PGH Foundation.
This article was originally published on The Conversation. Read the original article.