US medicines regulator the Food and Drug Administration (FDA) has approved a groundbreaking HIV prevention jab hailed as having the potential to quell the Aids pandemic.
But the moment has been overshadowed by the spectre of aid cuts, placing in doubt whether this breakthrough injection – lenacapavir – will get to the people who need it most.
Lenacapavir given in a twice-yearly injection stops HIV from replicating, protecting close to 100 per cent of people from developing the virus if they are exposed to it.
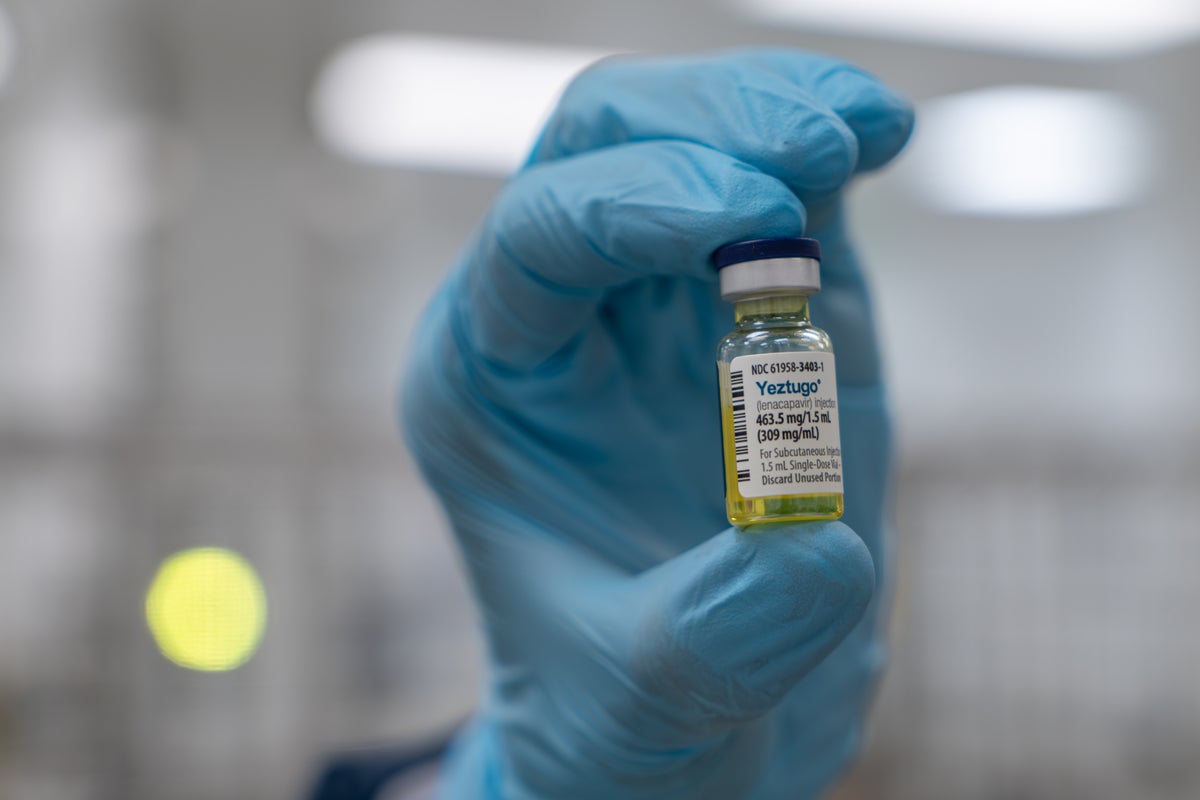
This approval is one of the last crucial steps to getting the drug, branded Yeztugo, out to patients. Although the FDA’s approval only applies to US patients, the World Health Organization (WHO) said it paved the way for its own recommendation of the drug and for approval in other countries.
Director of WHO’s Global HIV, Hepatitis and STI Programmes, Dr Meg Doherty described it as a “regulatory milestone” adding: “We are working with partners and national authorities to ensure lenacapavir reaches people who need it most – quickly, safely and equitably.”
Researchers have raised concerns that, amid aid cuts, the jab will be too expensive to be taken up by lower-income countries.
Gilead – the drugs company producing lencapavir – did not make public the cost of each dose to global funders but it announced a US price of $28,218 per year for each patient.
“If this game-changing medicine remains unaffordable, it will change nothing,” said Winnie Byanyima, executive director of the United Nations’ Aids agency, UNAIDS. She called the approval of lenacapavir a “breakthrough moment” adding the jab, “could be the tool we need to bring new infections under control – but only if it is priced affordably and made available to everyone who could benefit.
“UNAIDS has seen research that lenacapavir can be produced for just $40 per person per year, falling to $25 within a year of roll out. It is beyond comprehension how Gilead can justify a price of $28,218.”
Dr Andrew Hill, a pharmacology research fellow at the University of Liverpool, worked on the research which found lenacapavir could be provided for as little as $25, including a 30 per cent profit margin.
“Scientifically, it's a great moment that we have a drug which has been judged to be safe and efficacious by a leading regulatory authority in the world,’” he said. “Public health-wise and in terms of the epidemic, it's tragic because the drug is so expensive that it's not going to get used”.
It is also unlikely to be affordable in the UK, he said, despite government promises to end new cases of HIV in England by 2030.
A Gilead spokesperson said, “Yeztugo is priced in line with existing branded PrEP [pre-exposure prophylaxis] options. We are working to make Yeztugo accessible for anyone who needs or wants it and expect to see broad insurance coverage in the US.
“We’re taking unprecedented actions with urgency to plan for access to lenacapavir for PrEP globally—particularly in low- and lower-middle-income countries where the need is greatest.”
Gilead signed agreements with six pharmaceutical companies in India, Pakistan, Egypt, and the US to allow them to make generic versions of the drug in order to increase supply and drive down the cost of the jab. This will take some time.

Gilead also agreed to sell enough doses of the jab to protect at least two million people over three years in lower-income countries. These would be paid for by global funders led by the US President’s Emergency Plan for Aids Relief (Pepfar) and the Global Fund to Fight Aids, Tuberculosis and Malaria.
However, The Independent reported earlier in the month that these doses are now at risk because of US funding cuts.
A significant chunk of the money to fund the doses of lenacapavir was set to come from the US-led global Aids response programme, Pepfar, as well as the Global Fund whose biggest donor was the US. This funding is now uncertain.
Figures previously reported by The Independent suggest President Trump’s slashing of foreign aid has derailed the projected end of the Aids pandemic and could lead to four million extra deaths by 2030.
“It does feel like this thing that could help us end the epidemic sooner is suddenly receding in the chaos,” said Prof Linda-Gail Bekker, whose trial demonstrated lenacapavir’s effectiveness.
The aid-funded doses are thought to cost much less than the US list price of almost $30k but still roughly five times more expensive than Dr Hill believes is necessary.
And they are in an initial pilot phase, he said: “We need to get into a different level where we're giving lenacapavir to tens of millions of people”.
This is even more important as aid cuts are slashing the HIV prevention budgets of governments across Africa, he said.
“We're in this crazy position where we have a brand new highly effective vaccine-like drug and actually we will probably see the epidemic get worse over the next four years.”
This story is part of The Independent’s Rethinking Global Aid series
Watch: Smoke pours from Israeli hospital heavily damaged by Iran missile
North Korea will send 5,000 military construction workers to Russia, says Kremlin
India and Canada restore ambassadors as Modi and Carney meet at G7
Watch as the first flight of Israelis stranded abroad after Iranian strikes lands
Deadly Russia drone attack hits residential building in Kyiv with 14 killed
Trump claims ‘big stuff is happening’ as he leaves G7 summit early






