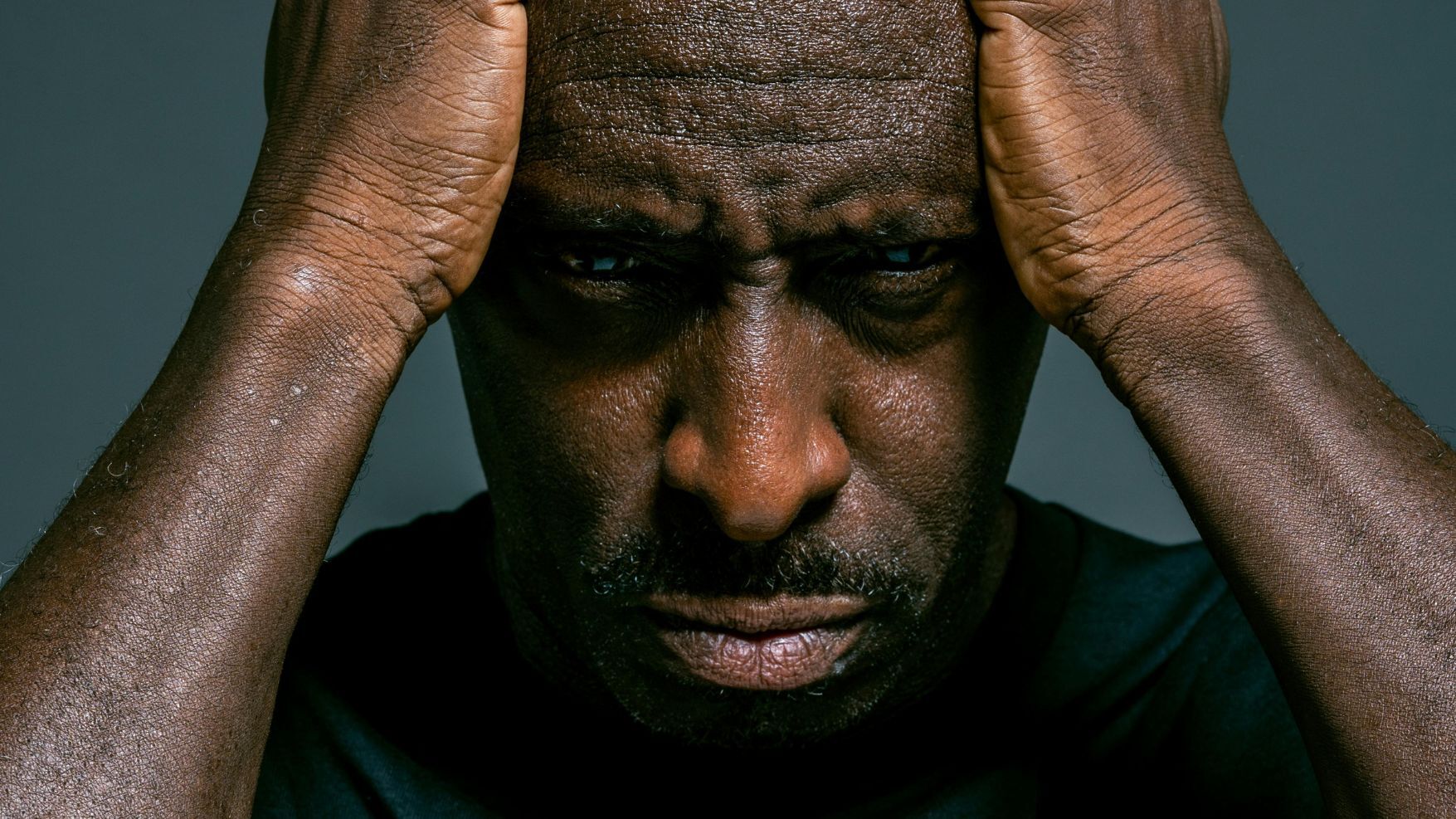
Mental health statistics today are certainly staggering, with 90% of Americans declaring a mental health crisis in the U.S. in 2022.
There are two classifications for mental illnesses: Any Mental Illness (AMI), which encompasses all recognized mental illnesses, and Serious Mental Illness (SMI). Combined, they affect 106 million people in the U.S., with the National Alliance on Mental Illness (NAMI) reporting that mental illness affects more than one in five adults today.
As we progress in 2026, it is important to understand the state of mental health today so we know how best to address the challenges facing this widespread – and growing – community. Based on the latest studies and research, these are the greatest mental health trends affecting Americans today.
2026 Mental Health Trends
Today’s latest studies and data show that mental health remains a driving issue in the daily lives of many Americans.
Research highlights several key trends.
Widespread Mental Health Illness
Between 2021 and 2024, there was no significant increase in mental health rates. However, individual well-being has decreased so much that the U.S. ranks 23rd among nations.
Leading conditions among U.S. adults include anxiety (19.1%), Major Depressive Disorder (15.5%), substance abuse (8.1%) and Post-Traumatic Stress Disorder (4.1%). Mental health rates are highest for females, as well as lesbian, gay and bisexual individuals.
By demographic, Non-Hispanic Native Hawaiian and Pacific Islander individuals ranked the lowest for mental health, Non-Hispanic Multiracial individuals (35.5%) ranked the highest, followed by Non-Hispanic American Indian or Alaska Native (25.9%) and Non-Hispanic White (25.1%) individuals.
Still, no one group is immune to mental health challenges, showing that many today are struggling for greater wellness.
Today’s Stressors to Blame

With all of the stress in today’s life, it is no wonder that mental health continues to be an issue.
A 2024 American Psychiatric Association (APA) poll revealed that anxiety is on the rise, with 43% of adults experiencing more anxiety than the year before (up from 32% in 2022).
“What stands out now is that the stress hums along, rather than fading away like everyday strain,” observes Amanda Ferrara, LMFT, of Ocean Recovery. “Our nervous systems are locked in overdrive, formed by news of economic pressure, political theater and threats of violence. Without it, we see anxiety, irritability, sleep problems, and a general difficulty managing moods.”
There are many reasons why the mental health of so many Americans is being affected, but the APA study highlighted three driving factors.
- The economy (77%),
- The U.S. election (73%),
- Gun violence (69%)
“From a neuroscience perspective, the current mental health landscape reflects sustained cognitive and emotional load on the brain rather than isolated stress events,” explains Dr. Ramon Velazquez, PhD, of Mind Lab Pro. “Prolonged exposure to uncertainty, social threat, and sleep disruption affects attention, memory, and emotional regulation by altering stress hormone signalling and neural plasticity.”
This can have long-term effects, he says. “Over time, this reduces cognitive flexibility and increases vulnerability to anxiety, depression, and burnout, particularly in younger brains that are still developing regulatory circuits.”
Youth, in particular, are plagued by a specific set of issues, including youth drug overdose deaths and gun violence.
“Young people can't help but notice that there is a mass shooting every single day in the United States,” says Dr. Owen Muir, a psychiatrist and chief medical officer at Radial. “We have now crossed another unfortunate Rubicon – we now have students surviving that one, but multiple school shootings in their lifetime.”
“The reality that these have not been stopped proves to young people who are worried that nobody cares... that the adults in power care more about their political careers than they do about stopping violence against children.”
Many respondents also said that stress (53%) and sleep (40%) were major contributing factors to their mental health.
“Chronic stress raises cortisol, making us more anxious, less sleepy, and depressed,” explains Kelsey Pabst, a Registered Nurse & Medical Reviewer at Cerebral Palsy Center. “Increasing symptoms of panic and physically-based stress reactions can be traced back to breaking news immediately spread via the internet and social media. Unrelenting threat perception leaves the nervous system in a ‘perpetual high alert.’”
Mental Health in Children Remains a Priority

Encouragingly, new research shows that mental health in children is improving.
A report from Mental Health America shows that major depressive episodes (MDEs) within youth ages 12 to 17 decreased from 18.10% in 2023 to 15.40% in just one year later. Additionally, suicide ideation dropped, with 12.30% of youth within the same group reporting suicidal thoughts in 2023, but just 10.10% in 2024.
Still, the Kaiser Family Foundation reports that between 2011 and 2021, feelings of sadness and hopelessness increased from 28% to 42%. Female and LGBT+ adolescents were shown to have higher rates of anxiety and depression.
This can be due to several reasons, with adolescents citing bullying (34%), emotional abuse by a parent (17%) and neighborhood violence (15%) as reasons between 2021 and 2022. Extended screen time can also be harmful to overall mental health and well-being.
By 2024, 32.2% of young adults ages 18 to 25 reported mental illness, encompassing nearly 12 million people.
However, today’s youth is being proactive about their health. NAMI reports that about half of minors ages 6 to 17 with a mental health disorder received treatment in 2024. The year prior, more than a quarter of high school students had reported experiencing poor mental health within the previous 30 days; for LGBTQ+ high school students, it was more than half.
Suicide Ideation Persists
Every 11 minutes in the U.S., one person dies by suicide. In 2024 alone, suicide ideation affected over 14 million adults.
Almost half of those who die by suicide were previously diagnosed with a mental health condition, although family, friends and medical professionals say the number is far greater, with 90% of people who commit suicide previously suffered symptoms of mental health illness, regardless of an official diagnosis.
Suicide levels continue to rise in 2026, giving the U.S. the highest death rate among 10 peer nations. It affects all ages, too; in 2021, suicide was the second leading cause of death among those ages 10 to 14 and 25 to 34. While 20% of high school students seriously contemplated suicide in 2023, the number was more than double (41%) for LGBTQ+ students.
Rates have been shown to be the highest for American Indian, Alaska Native and White adolescents. Males are almost four times more likely to die by suicide than females, although females have a higher rate of suicidal thoughts and suicide attempts.
The LGBTQIA community highlights a crucial need for added support. Transgender adults are nearly nine times more likely to commit suicide during their lifetime than the general population, while LGBTQ+ high school students are more than three times more likely to attempt suicide compared to their heterosexual, cisgender peers.
“Members of the L.G.B.T.Q.+ community report very high rates of anxiety, depression, and exposure to trauma related to stigma and stress,” explains Nurse Pabst. “Based on research, these groups show up late and unwell, rather than early on in crisis.”
Ferrera agrees, saying, “Many meet the criteria for an anxiety or depression diagnosis, yet never receive any kind of structured therapy. In the absence of timely intervention, those symptoms can turn into deeply rooted patterns that increase risk for substance use and suicidality.”
Substance Abuse Still a Contributing Factor
Substance abuse also remains a driving factor in today’s mental health challenges.
“The overlap between mental illness and substance use is a huge challenge,” says Bonnie Lambert, LMFT, of Crestview Recovery. “Many people report that they are simply using substances recreationally when, in fact, they are self-medicating anxiety, trauma, insomnia or emotional numbness. Without treatment that addresses both mental health and addiction at the same time, relapse is almost inevitable, and sustained long-term recovery becomes nearly impossible.
“Co-occurrence is common as substance use and mental health issues can share common underlying factors, including genetic vulnerabilities and exposure to high levels of stress or trauma, particularly in childhood,” shares Cort M. Dorn-Medeiros, Licensed Professional Counselor, Addiction Specialist and Associate Professor at Lewis & Clark College.
“Additionally, people who struggle with mental health issues may use substances to help cope with distressing symptoms. Likewise, chronic use of substances may trigger underlying mental health issues. Depression, anxiety, schizophrenia, and personality disorders have some of the highest rates of co-occurring substance use problems.”
Drug overdose is a main factor affecting adolescent mental health, with deaths more than doubling from 2018 to 2022 and especially impacting Hispanic and Black adolescents. Adults suffer from substance abuse issues, as well, with substance use disorder (SUD) affecting over 46 million people.
“These are people ripped out of our lives abruptly,” says Dr. Muir. “More and more of us know people who are dying young, and that causes a tremendous amount of grief. We don't have great social structures around coping with large-scale grief, and so people are left to try to make sense of something that doesn't make any sense. For people who are vulnerable to depression, anxiety, or other psychiatric disorders, you can imagine that these stressors weigh heavily upon them.”
However, there is encouraging news. For the first time since 2018, the number of deaths due to overdose actually decreased in 2024.
This is something that Mental Health America says is likely due to federal and state developments in drug treatment and prevention strategies. Some states have been better than others; Utah, Indiana and New Jersey ranked among the best, while Rhode Island, Colorado and the District of Columbia ranked at the bottom. Rural areas continue to be plagued by limited resources and support, likely due to budget constraints and lack of accessibility.
Access to Care Remains a Challenge
Rural areas admittedly have a harder time providing resources for their communities, but there is also a great disparity among the states.
A Mental Health America study found that New York, Hawaii, and New Jersey offered the best access to mental health care, while Alabama, Arizona, and Nevada had the worst. It is the second year in a row that Nevada and Arizona bottom the list. For youth, the District of Columbia, Vermont and New York ranked the best, while, again, Arizona, Alabama and Nevada scored the worst.
This is something that Lambert has seen personally during her time at Crestivew Recovery. “In the U.S., timely treatment might not be available outside of urban centers because huge numbers of people live in ‘mental health deserts’ with months long wait lists, specialists who don’t take insurance, or fees that require a second mortgage.”
It especially affects minors. Today, more than half of Americans see youth mental health illness as a crisis, with few adolescents receiving the therapy they need. Over two-thirds of U.S. public schools report an increased need for student mental health services at school, but nearly half said they lack the ability to adequately meet their students’ mental health needs. In 2021 and 2022, only 20% of teens reported receiving mental health therapy, and just 14% reported taking prescription medication.
“Teens are grappling with rising rates of anxiety and depression, but a vast majority do not receive assessments because of stigma and lack of access to child psychiatry,” Nurse Pabst shares. “Schools usually spot the problems before healthcare does, which leads to severe symptoms once they are seen. Early screening in schools and pediatric offices might help catch these issues earlier.”
However, even those who want mental health services may not be able to obtain them, with one-third of respondents not receiving the care they need. Cost was the driving factor, with shame and stigma following closely behind.
“Men and L.G.B.T.Q.+ adults in particular felt like they needed to deal with it on their own, or that they weren’t comfortable showing their emotions,” Ferrera explains. “They are being identified as stressed at higher rates at the same time that they lack consistent access to care.”
However, getting that care is not always so easy, as there is also an ongoing issue with medical professionals. In 2022, 60% of psychologists reported no availability for new patients, creating a serious accessibility issue for those seeking help. This is coupled by the fact that over 120 million people live in a designated Mental Health Professional Shortage Area.
Treating mental illness is not cheap, with estimates at $282 billion annually.
“It’s not just that the prevalence is so high, but that there aredelays to care,” says Nurse Pabst. “If we can focus more on primary care and do more early screening, a lot of the emergencies would be prevented.”
It has prompted mental health providers to create and embrace new strategies to improve availability, such as telehealth appointments with online messaging and chat support. Medical professionals report that it has made a particularly significant difference in community clinics and on college campuses.
“Telehealth services can close the gap for ongoing support with follow-ups, medication management and educational outreach,” explains Lambert, “but only when combined with trauma-informed care that treats the person as a whole and involves family members and pragmatic skills for recovery.”
Overall, Nurse Pabst says, telehealth is working. “Those seeking therapy or psychiatry were often faced with waits lasting months. Telehealth has made iteasier for rural patients to get care, for working parents to avoid time away from their jobs and kids and for teens who might be reluctant otherwise.”
“No-show rates are down, and follow-ups have improved with virtual visits that help close an enormous care gap.”
Bottom Line
Mental health does not discriminate. It affects adults and children alike, touching Americans from all walks of life and all corners of the country.
With 83% of American households negatively impacted by untreated mental illness, it is an issue that commands attention.
“What is encouraging is that the brain remains highly responsive to intervention when support is timely and evidence-based,” says Dr. Velazquez. “Access to care, whether in person or through telehealth, supports neuroplastic changes that improve emotional regulation, impulse control, and resilience. Early treatment, sleep stabilization, reduction in substance use and skills-based therapy are not just psychological supports but biological interventions that help restore healthier brain function and long-term mental performance.”
Continued prevention programs, combined with additional professional training and cooperation with national associations, are expected to help address the mental health crisis in America going forward, giving adults and youth alike the chance to live a happier and healthier life.







