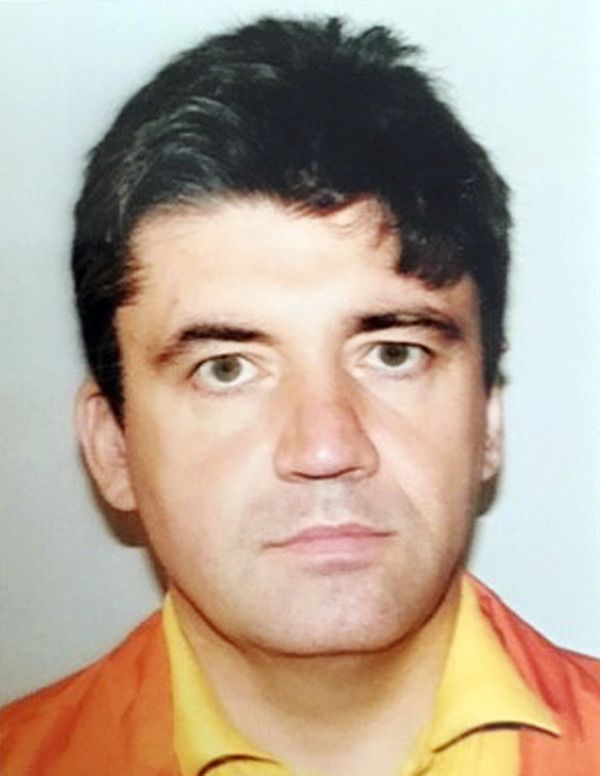
Time and time again, public health officials say childhood obesity is a serious problem in the United States. Dr. Christopher F. Bolling, a retired pediatrician and volunteer professor of pediatrics and the University of Cincinnati College of Medicine, told Salon he’s personally seen childhood obesity rise in the U.S. through the culmination of his own practice, which he started in the late 1980s.
“I have seen the obesity epidemic from the beginning,” Bolling said. For all of its limitations as a metric for individuals, he elaborated, body mass index (BMI) can provide insights into population patterns. “The percentile that's really exploded, has been that greater than the 99th percentile, the kids with severe obesity,” he said. “And we see illnesses that I never saw in kids in my training in the '80s, like type 2 diabetes, which is a weight-related version of diabetes.”
Bolling is part of a task force with the American Academy of Pediatrics who recently updated its own guidelines on childhood obesity prevention, or what the authors refer to as the “promotion of healthy lifestyle.” In the report, Bolling and his colleagues focus on a variety of behavioral interventions for each stage of childhood, including focusing on good sleep and limiting screen, all of which can enable a more sedentary lifestyle that can become problematic later in childhood.
Bolling also acknowledged that there are systemic issues at play when it comes to childhood obesity — like school districts cutting back or eliminating their physical education programs. Still, it’s a concern of many pediatricians and he believes that the pediatrician can play a role in promoting preventative measures in childhood.
“We worry about obesity as an illness and as a chronic disease,” Bolling said. “And what we're trying to do is we're trying to head off that chronic disease, so we're not just trying to prevent obesity, but we’re trying to prevent all the things that come along with it.”
The report comes nearly a year after the much-criticized childhood obesity treatment guidelines were released in 2023, which included a mix of recommendations, ranging from behavior and lifestyle treatment to anti-obesity medication and bariatric surgery. Specifically, AAP said doctors should offer weight loss drugs to adolescents diagnosed with obesity at age 12 or older. Severe obesity is defined as a BMI of 120% of the 95th percentile, or roughly the 99th percentile, for age and sex.
Judging from headlines at the time, these suggestions alarmed eating disorder specialists. Yet over a year later, anecdotal data shows that those guidelines are likely being followed as more reports surface about adolescents and teens being prescribed anti-obesity drugs like Ozempic and Wegovy, which has the generic name semaglutide.
Research has shown medications like semaglutide can be effective in treating adolescent and teenage obesity. For example, one study of 12 to 18 year olds found that those with severe obesity had a greater reduction in BMI than lifestyle intervention alone, when lifestyle interventions were coupled with a once-weekly 2.4 milligram dose of subcutaneous semaglutide.
While the AAP prevention guidelines didn’t mention anti-obesity drugs, it does resurface the debate on adolescents and teens taking semaglutide. Bolling said he thinks they are an option pediatric patients should be aware of when confronted with severe obesity, and emphasized that the guidelines that received pushback were based on physicians reviewing thousands of articles of data.
“We were all very impressed with how the data showed that medication for kids who have comorbidities, who have hypertension, diabetes, sleep apnea and the effect that medication had in treating the weight,” he said. “The data was saying to us, this works, and if you ever have something that works, you can't suppress the data on it — it’s something patients deserve to know about.”
He emphasized that it’s not meant to be used in adolescents and teens in “isolation” or for “cosmetic reasons.”
“This option is for people who have severe obesity,” he said. “Who have physiologic changes that are causing them to get life-shortening illnesses.”
Kimberly Vered Shashoua, a therapist who works with young adults with eating disorders, told Salon she is concerned about adolescents and teens being prescribed anti-obesity drugs from a mental health perspective, despite some anecdotal stories on how the medication improves youth mental health.
“I think it's really helpful to think about what makes people fat,” Shashoua said. “There are lots of longitudinal studies, there are lots of animal studies, that stress and especially experiencing trauma, will increase fat accumulation.”
Shashoua said society is “treating fatness” without considering what’s driving it in America.
“Is the reason that you're seeing the mental health improvements [with youth on anti-obesity drugs] because society just has such contempt for fat people?” Shashoua asked. “It is a lot harder to have societal changes.”
Shashoua said treating obesity with anti-obesity medication is a reflection of America’s “bootstrap, culture, individual, ritualistic solution," adding that dieting is a risk factor for developing eating disorders. “Weight cycling is a huge factor for not only having your weights and up higher, so if you lose a lot of weight, it's likely that you will end up at a higher weight than when you started and there are a lot of negative health effects that happen from weight cycling.”
In January, a report came out that found 1 in 10 teens worldwide have used so-called “budget Ozempic” laxatives and other risky weight loss products to lose weight. Since the drugs aren’t meant to be used to treat obesity in teens, the study’s authors expressed concern that this trend could pose immediate and longer-term health risks.
“These findings were surprising,” Dr. Natasha Hall, a co-author of the study, told Salon. “Even though to some, the percentage might look low, it's actually affecting a huge number of American children.”
When people look for solutions, Shashoua said: “We need to look at research that controls for anti-fat bias.”
When asked about fat-bias, Bolling said he agreed that there is too much weight stigma bias in the United States.
“People who have excess weight, that's not their fault,” Bolling said. “You don't blame people who have asthma for having asthma. We need to quit blaming people for their obesity and quit blaming people for something that is a combination of all sorts of things — genetics, environment, mental health issues.”
At the same time, Bolling said, severe obesity can lead to various comorbidities if it’s ignored and that’s a concern for pediatricians. The goal for pediatricians, he added, which touches on the preventative guidelines, is for patients to be the “happiest and healthiest patient you can be.”
“And that is different for different people,” Bolling said.