When I walked into work last October, the ER was in its usual state of organized chaos, with EMTs lined up in the ambulance bay and patients already crowding the hallways.
Not long after I sat down at my desk, I heard a commotion. I turned my head towards the noise and caught a glance of a youngish, medium-statured man. He was yelling obscenities and dragging his feet as security guards led him to the exit.
Around midnight, I overheard the head nurse pleading on the phone, “You really can’t do anything? We need an officer parked in front of the ER!”
The same man had called the hospital’s operator and made threats to return with a gun.
I called the police myself and did my best to exude the confidence of a doctor in charge, but their answer remained the same. The officer explained they had checked the man’s apartment for firearms, but that was about all he could do. When I insisted that the police either send us reinforcements or keep an eye on the would-be shooter, the officer said flatly, “he said he was sorry.”
I felt dumbstruck. Would the officer have been so nonchalant if the same man had threatened to terrorize a school or an airport? Why should our lives matter less? What about our patients?
I immediately discharged everyone who was well enough to go home and gathered my nurses for a huddle.
“When he comes, we will only have a couple of minutes. The patients who can walk, we take with us. The ones who can’t, we close their doors and throw cart, stretcher, whatever we can find in front. We have to get to safety before he breaks into the main ER. Don’t dally,” I said.
“He left through the ambulance bay, so he knows it’s there,” one of the nurses chimed. She was right. The last thing I’d want was to come face-to-face with the shooter while trying to make my way out.
“What about the med room?” I asked.
“No, the door has glass. He can just shoot through it,” another nurse retorted.
“Right! Then, how do we get out?”
“The back door,” they said in unison.
This huddle was our first time gathering to discuss the matters of our life and death, yet it did not feel spur-of-the-moment. All of us have been thinking about this exact scenario for months.
I first noticed the shift about a year ago. Our New York state patients were accustomed to modern facilities and efficiency, and they did not always adjust well to the new realities of the pandemic. Some dealt with their disappointment by pacing, yelling, and cursing until they got their way. Others with more clout called administrators they had on their speed-dial.
Gillian Schmitz, the president of the American College of Emergency Physicians, had a similar experience in July 2018. She was working an overnight shift at First Choice ER in Texas when a man came in at two o’clock in the morning with a strange request. He wanted to see the cat scanner and tour the facility.
She suspected that he might be looking for narcotics and other pharmaceuticals on site. The man left but then pulled out a gun outside the facility and shot a person across the street. “I was terrified that he was gonna come right back,” said Schmitz.
When the police arrived 30 minutes later, they told her: “Well, we can’t stay here all night. We don’t know where this guy is. He might come back, but he might not. We’ve got other people to take care of.” Thankfully, the shooter did not return. “It is sort of an unsaid rule,” Schmitz says. “People think that this is part of our job, that part of being frontline providers is to bear the brunt of this [violence].”
Such incidents have been on the rise in the past decade, but even more so since the pandemic. Last year, when 7,411 adults were surveyed, it transpired that healthcare workers were 50% more likely than others to have been harassed, bullied, or hurt as a result of Covid-19. “Physicians are unfortunately fighting a two-front war,” noted Susan R Bailey, the 175th president of the American Medical Association.
In response, a hospital in Missouri planned to distribute 300 panic buttons to its staff. Another hospital in Ohio implemented Code SOS, an ER protocol to quickly de-escalate when patients begin showing signs of agitation.
Lawmakers, too, tried to address this problem. In April, the US House of Representatives passed HR 1195 – the Workplace Violence Prevention for Healthcare and Social Service Workers Act – but the changes may not be coming fast enough to stop the exodus of burned-out healthcare workers.
•••
I rarely worried about my physical safety until an incident over the summer. During a night shift, I found one of our nurses visibly upset. When I asked her what happened, she told me that a patient pulled out a knife and tried to attack her.
Triage, once a routine process to assess the patient’s acuity, evolved into a dangerous task since it’s come to include questions about Covid-19 symptoms, exposure, and vaccination. Nurses now had to brace themselves for unpredictable reactions.
“Tensions are higher. People’s fuses are a lot shorter. The pandemic definitely accelerated that,” Schmitz noted. “It’s like the perfect storm when you combine increased wait times with politicization of everything.”
Tensions finally came to head in September when a disgruntled patient returned to our ER with rocks gathered from the hospital garden. The first one broke through the glass of our front entrance. He then threw the rest directly at staff members manning the front desk. He then targeted the entrance to the main ER. To prevent him from charging through, one of the doctors used his body as a shield against the door. The police eventually arrived and arrested him, but the man returned two weeks later and made additional threats.
I learned such issues extend beyond my workplace when I spoke to Claire, an ER nurse at a large academic center in Manhattan. I showed up at her apartment in late November and was surprised to find her in a splint. She explained a patient grabbed her while she was trying to attempt an IV. She could not yet move or bear weight without pain.
The most recent National Nurses United survey, published in September 2021, showed that Claire isn’t alone. Nearly a third of nurses (31%) reported that workplace violence recently increased. Claire and I agree some root causes are more obvious than others. With multiple waves of Covid, patients were seeking medical care in unprecedented numbers while restrictive visitor policies, crowded spaces, and increased staff turnover continued. Moreover, misinformation about the virus, fear of catching Covid in hospitals, and limited mental health resources have only intensified patients’ distrust of the healthcare systems.
But there were aspects of the public’s misplaced anger that we could not quite comprehend.
“People will walk into the ER, throw their garbage at you, and walk out. One nurse got dog poop thrown at her. They’ll just walk up to you, say ‘F you,’ and walk out. People just don’t understand. The homeless or the untreated mental health patients that are walking around with schizophrenia are my favorite ‘violent patients’ because they don’t have insight or capacity. Worse are entitled patients who come in and treat you like you’re not human.”
Even with her injury, Claire tried to return to work the next day; she knew her colleagues were already stretched thin. She asked her supervisor to assign her to a less physically demanding role, but her supervisor refused. She then had to navigate bureaucratic red-tape and passive-aggressive emails from risk management in order to report what happened.
Claire’s experience is hardly unique. Many institutions, reliant on patient satisfaction metrics for reimbursement from Medicare, tout the “customer is always right” mentality, and administrators discourage staff from reporting incidents of violence or harassment. A 2019 brief from the American Nurses Association cites “fear of being accused of inadequate performance or of being blamed for the incident, and fear of retaliation by the offender and or employer” as one of the causes of under-reporting.
At Claire’s year-end review, she received average marks despite her meeting and exceeding expectations. When she inquired as to why, her managers explained that everyone, including all of her colleagues who have been working overtime, received the same marks.
It then all made sense: average reviews meant the hospital did not have to pay out any merit-based bonuses. Claire left her job shortly after.
•••
Congressman Joe Courtney, one of the politicians behind HR 1195, continues to fight for legislative change because of men like Eugene Sausse. In 2019, Courtney received a text from his staff. Sausse, a staunch Republican and conservative, had driven straight from Louisiana to show up unexpectedly at the congressman’s Capitol Hill office. He had come all that way to discuss what happened to his sister.
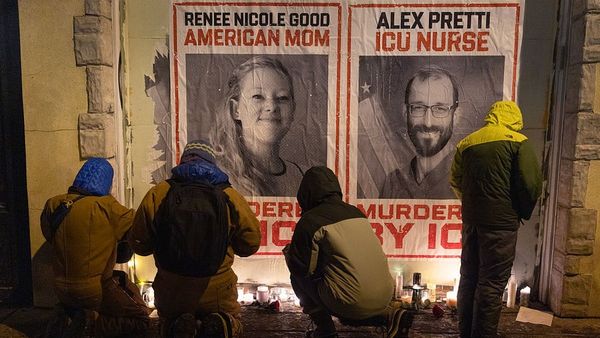
Lynne Sausse Truxillo worked as a nurse at Baton Rouge General Mid City Hospital when Jessie Guillory, a behavioral health patient, attacked her coworker. When Truxillo intervened, Guillory grabbed her neck and struck her head on the desk. She died five days later from complications from her injuries.
“Sausse was determined not to let this experience just slide,” Courtney recalled. “He really wanted something to change.”
Stories like Lynne’s were not new to the congressman. They’d come to him at home over the dinner table as his wife, a pediatric nurse practitioner, recounted her day. He sensed early on that violence against healthcare workers was a serious issue, but he could not rely on anecdotes to propose legislation. He needed data, which he did not have, since there were no central entities that kept track of incidences.
When he finally received national data in 2016, his concerns were confirmed. The rates of violence against healthcare workers were 12 times higher than rates for the overall workforce, while 70% of nonfatal workplace assaults in 2016 occurred in the healthcare and social assistance sectors. More alarmingly, these numbers were gross underestimates given that healthcare workers only reported their injury about 7 to 42% of the time.
National guidelines for hospitals do exist, but employers aren’t required to implement workplace violence prevention programs.
“We are never going to get real change without really putting something into law and establishing an enforceable standard,” Courtney said. “That’s what the bill seeks to do.”
HR 1195 passed in the House last April and is waiting to go to vote in the Senate, but groups like American Hospital Association are actively opposing it. In a letter sent to Courtney on March 23, 2021, vice president Thomas P Nickels cites “prohibitive cost” to “private entities” as a cause for objection.
•••
After the waiting-room attack in September, administrators at my hospital called multiple mandatory meetings about safety. Most of these meetings targeted staff behavior: was the assailant jostled awake too roughly? Did we personally hand him his discharge papers?
Two days after the shooter threat, we had another meeting, and one of my supervisors once again focused on staff behavior. “He was provoked,” he said multiple times. We had to do better because “society had failed him”.
Though I admired his intentions, I felt he wasn’t seeing the whole picture. After much hesitation, I forced myself to interject. “These things happen even if we do everything perfectly,” I finally blurted out.
The following month, another incident proved my point when a patient’s family member punched a staff member out of the blue. Witnesses agreed the assault was unprovoked.
After that, changes did come, albeit slowly. Over the next several weeks, physical reinforcements were made to the most vulnerable areas of our ER, staff re-trained, security added, a task force formed, and stones removed from the gardens.
With these improvements in place, we have not had another major event. Still, violence, burnout, and staff shortages continue to feed into each other, and sometimes one can observe the whole cycle play out in the microcosm of a single interaction.
On Christmas Eve, people swarmed the ER to receive their clean bill of health. It meant we saw double the number of patients with fewer than usual staff. At 7.05pm, I spotted one of our veteran nurses looking frantically for a Covid swab, which was becoming increasingly scarce. When she found one, she approached a large middle-aged man who had been pacing the hallways.
But before she could perform the test, he stomped his feet and began yelling.
“You know how long I’ve been waiting!” he dug into her. “This is ridiculous!”
The nurse told him calmly: “My shift ended. I was staying late to help you, but I’m gonna go home now.”
The patient’s tone immediately softened. “I’m sorry! Please, don’t go. Please do my swab!”
But her mind was made up. She was going home, and I wouldn’t have blamed her if she never came back.