When Dr Art Van Zee finally understood the scale of the disaster looming over his corner of rural Virginia, he naively imagined the drug industry would be just as alarmed.
So the longest-serving doctor in the struggling former mining town of St Charles set out in the early 2000s to tell pharmaceutical executives, federal regulators, Congress and anyone else who would listen that the arrival of a powerful new opioid painkiller was destroying lives and families, and laying the ground for a much bigger catastrophe.
Two decades later, as Van Zee surveys the devastation caused by OxyContin and the epidemic of opioid addiction it unleashed, he is still in disbelief at the callous indifference to suffering as one opportunity after another was missed to stop what has become the worst drug epidemic in US history.
But the 76-year-old doctor is also shocked that the crisis has got so much worse than even he imagined as one fresh wave of narcotics after another dragged in new generations and drove the death toll ever higher.
“This region has been through a lot but the drug problem is the worst thing that’s ever happened in central Appalachia in terms of human cost and devastation to individuals and families. You’ve got all these families that came apart, children living with dysfunctional parents or went into foster care. Children who learned from their parents to take drugs from a young age. The devastation is going to go on for generations,” he said.

“It didn’t have to happen. There were so many missed opportunities. So many times it could have been stopped. Now, I don’t see how it ends.”
As it turned out, the drug industry was alarmed by Van Zee’s warnings, but not in the way he expected. It saw the doctor as a threat to profits and so from the very beginning, big pharma responded by working to discredit Van Zee and others like him who rang the alarm on high-strength opioids creating mass addiction.
Years later, there had been other opportunities to slow the crisis before it evolved from prescription pills to illicitly produced fentanyl and other drugs that together have claimed 800,000 American lives over the past quarter of a century with predictions of another million deaths by the end of the decade. But federal regulators and prosecutors failed to seize the moment.
Perhaps most disturbing of all, Van Zee said the US was still failing to learn the lessons of a uniquely American catastrophe to break the influence of corporate money over medicine, drug regulation and political accountability.
“I trace this back to OxyContin and the opioid problem because it brought this huge number of people in our region into the substance-using world, and for so many years good treatment wasn’t available. But now we’ve got methamphetamine, and fentanyl more recently. It’s much worse than I imagined it would ever be, and the lessons haven’t been learned.”
Van Zee first went to St Charles in the mid-70s as a young doctor volunteering to help out the struggling town in a sliver of Virginia poking like a finger to the west between Kentucky and Tennessee. He liked the place so much, he returned in 1976 and has stayed ever since working at its community health clinic.
St Charles and surrounding Lee county once thrived off the coalmines. Thousands of men worked at the largest of them, the Bonny Blue.
“Saturday night you couldn’t walk through town. It was shoulder to shoulder. They had hotels, grocery stores. It was full of life,” said Van Zee.

But by the time the new doctor arrived in town the mines were in retreat and the area struggled as incomes plummeted. Like other parts of Appalachia, distant coal barons got rich plundering the coal but left little behind to sustain the mining towns when the seams ran dry. Some in the region liken their history to the colonial exploitation of Africa and Asia.
After the mines closed in Lee county, the population in St Charles collapsed to the point where in 2022 the Virginia legislature removed the town’s charter because no one ran for office for two elections.
Many of those who remained were ripe for the plucking when the drug industry came pushing opioid painkillers in the late 1990s, and one drug in particular. OxyContin was so powerful it wasn’t long before it was known as “heroin in a pill”.
The mix of ageing laborers with worn-out bodies seeking pain relief and young people looking for escape turned out to be a rich market for big pharma.
Van Zee saw the first flickers of the coming epidemic in 1999 when patients began telling him about partners and children suddenly hooked on OxyContin. Soon the drug seemed to be everywhere.
The manufacturer, Purdue Pharma, was running one of the biggest marketing campaigns in the drug industry’s history to persuade doctors to prescribe OxyContin on the grounds that it was less addictive and more effective than other opioid painkillers. Neither claim was true. In fact, OxyContin’s high narcotic content made it more dangerous.

Most American doctors had little training in opioids for pain management so they tended to accept at face value the Purdue sales reps’ claims even though they had no medical training at all.
By the time Purdue came knocking on Van Zee’s door, he knew better. Still, he was certain that if the drug maker only knew the situation on the ground it would do the right thing. He wrote to the company and to the Food and Drug Administration which regulated big pharma.
When his letters were ignored, Van Zee turned up at meetings where Purdue was using doctors to promote OxyContin and challenged the speakers. He kept writing to the company comparing the growing catastrophe its drug was causing in parts of Appalachia to the “sentinel areas” of New York and San Francisco at the beginning of the HIV/Aids epidemic.
By 2001, the situation was so bad in Lee county that Van Zee organised a town hall meeting in St Charles and began a petition to the FDA to have OxyContin withdrawn from sale.
“There were 800 people in our little high school auditorium over the OxyContin problem because it was painful, it was acute. There was nobody untouched,” he said.
Finally, Purdue agreed to a meeting where Van Zee proposed the company send warning letters to doctors across the country alerting them to rising OxyContin addiction and death, and end the marketing of the drug except for those who really needed it, like cancer patients.
Purdue did none of these things. So Van Zee pressed the FDA to restrict OxyContin to treatment of severe pain. The agency called a hearing.
By then, OxyContin was earning Purdue Pharma more than $1.5bn a year and making its owners, the Sackler family, extremely rich. Neither had any intention of letting a small-town doctor and other critics of their drug get in the way of booming profits.
The industry lined up heavyweight pain specialists in its pay to defend the mass prescribing of opioids at a rate far beyond any other country. One of the specialists who gave evidence was taking money from 16 pharmaceutical companies including Purdue.

Van Zee made his case at the FDA meeting when the public was permitted to speak but by the end of the two-day hearing it was clear to him that there was no sense of urgency on the part of the federal agency.
“If the FDA had got on a bus and come down to central Appalachia or gone up to Maine and spent a couple of days talking to people in communities about what was going on maybe they would have understood more. They just didn’t understand the scope and the tragedy of it,” he said.
Van Zee concluded the FDA was far too close to the drug industry, with agency officials often moving to jobs at big pharmaceutical companies, to be able to regulate it properly.
So Van Zee tried Congress. Committees of both houses held a series of hearings in the 2000s.
“There has never been anything to compare to the epidemic of drug abuse and addiction that we have seen the last three years with OxyContin,” Van Zee told senators.
Purdue’s head of research and development, Paul Goldenheim, spoke for the company. Goldenheim’s strategy was to absolve OxyContin by blaming the addicted as morally deficient “drug abusers”.
Senator Christopher Dodd, an influential Democrat who represented Connecticut, where Purdue was headquartered, accused Van Zee of harbouring an “exaggerated fear” of opioids causing addiction and parroted the company’s line that the problem was people not OxyContin.
But Van Zee had a prescient warning for Dodd and the rest of the Senate committee.

“Over the next decade we will find out that there has been a lot of unfortunate errors made about how much we have done with how little knowledge we have had to do it,” he said.
Deaths did indeed continue to surge, alongside other human costs.
Van Zee has a map of those parts of his region where OxyContin was most widely prescribed. He lays over it another map of the highest rates of children taken into care during the same period. They closely match.
In the early years of the opioid crisis, the number of children taken into care or fostered quadrupled in Lee county.
“That’s just a fraction because so many of the children didn’t go into foster care but got taken in by grandparents or cousins. They weren’t registered with official statistics,” he said.
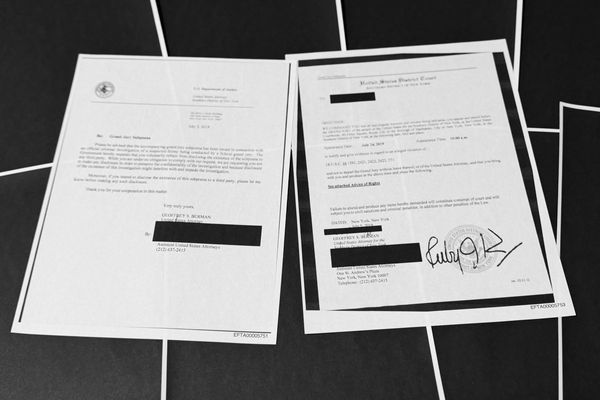
Van Zee and others campaigning to restrict sales of OxyContin found new hope when the US justice department indicted Purdue Pharma and three of its senior executives in 2007 for deceptively marketing the painkiller as safe than similar drugs.
Was this the moment when Purdue and other companies, such as Johnson & Johnson which had jumped on to the opioid bandwagon, would finally be forced to stop selling the “heroin in a pill”?
Again, big pharma slipped away. Prosecutors negotiated a deal in which Purdue paid a large fine but was allowed to go on selling OxyContin largely unfettered, and a deal was struck for its executives to plead guilty to misdemeanours and avoid prison time.
The flow of OxyContin was undisturbed and opioid prescribing continued to escalate.

Van Zee has little time for Purdue Pharma and the Sackler family’s attempts to downplay their responsibility for the cynical and calamitous push to sell OxyContin to people who didn’t need it. The company that fired up and fuelled the opioid epidemic is now bankrupt. The US supreme court will decide whether a deal that allowed the Sacklers to pay billions in restitution, while still holding on to a good chunk of their ill-gotten gains, is legal.
But Van Zee is concerned that a narrative has taken hold of Purdue and the Sacklers as the only bad apples and that has resulted in a failure to learn the real lessons of how the big pharma executives were able to behave like what one West Virginia mayor called “drug dealers in Armani suits”.
“It’s so easy to demonise Purdue and the Sacklers. I agree that what they did was terrible. I think a number of them should be in jail. But I’ve thought for some time that the issue behind it all is the structure of the system,” he said.
“They were able to do it within a system that allowed and permitted such heavy pharmaceutical influence on the medical professional, on regulation, on Congress. We’ve got to look beyond the Sacklers to be able to change the system somehow.”
Van Zee points to the huge amount of money spent on marketing drugs in ways not seen in other countries, including television advertising of prescription medicines that is permitted in only one other country, New Zealand. He also wants to break the link between the medical profession and big pharma’s money.
Van Zee recalls attending a talk by Russell Portenoy, a doctor who was hugely influential in breaking down caution about the risks of opioid addiction and steering physicians toward mass prescribing of painkillers. He was struck by the amount of funding Portenoy received from a raft of drug companies, including Purdue, for research.

“He spoke with some pride about pharma paying him. So if you’re a primary care doctor and don’t know much about this area, and you hear an expert in the field with 13 letters after their name, you can’t but help be influenced by the message. But that message was influenced by all those pharmaceutical companies who were paying him,” he said.
Years later, Portenoy recanted his claims for the safety of opioids, and admitted that research money from big pharma influenced outcomes, but by then the damage was long done.
In 2019, separate research by Journal of the American Medical Association and the National Bureau of Economic Research demonstrated the correlation between those parts of the US targeted for drug company sales drives and a rise in opioid deaths.
In addition, the industry co-opted federal regulators, a medical establishment too often focused on the interests of doctors over patients, and indifferent and corrupted politicians more willing to listen to the word of lobbyists than physicians.
Hospital corporations and health insurers bought into the push to opioids because it was in their financial interests. Drug distributors, among the largest companies in the US, delivered opioid pills by the millions into the heart of the epidemic without any attempt to fulfil their legal, let alone moral, obligations to monitor and report glaring evidence that rogue pharmacies were feeding and profiting from addiction.
President Donald Trump appointed an opioid commission which spread the blame for what it called the US’s “national nightmare” to include the public institutions supposed to protect Americans. Foremost was the FDA, which opened the door to the wide prescribing of powerful opioids in the first place and then made no real effort to close it again.

The FDA, its independence increasingly compromised by its dependence on income from the pharmaceutical industry, consistently subordinated public health to the financial interests of the drug makers by permitting ever more opioids on to the market.
In 2019, Dr Raeford Brown, then chair of the FDA’s committee advising the agency on whether to approve new prescription opioids, warned that its failure to apply the lessons of its role in the epidemic would perpetuate the crisis.
“We’re going to revisit an opioid problem in five years and 10 years and 15 years and 25 years. We can’t just make believe that things are going to go away,” he said.
Van Zee laments that too many doctors are comfortable with the cosy relationship between the medical profession and big pharma.
“There’s just this tiny thread in medicine of people saying we have to separate ourselves from the industry. When I went to medical school, the usual thing was for drug companies to give medical students black bags and stethoscopes. There was a small number of us that wouldn’t take that,” he said.
Van Zee supported the “No Free Lunch” movement which sought to break the link between the drug industry and medical training for doctors. Big pharma has a large say in the writing of training manuals which sometimes had the effect of pushing their drugs over other more effective treatments, one reason Americans consume prescription medication at a much higher rate than other countries.
“They called attention to the issue but it’s always been a minority voice. By and large the profession is quite willing to take the free lunches,” he said.
Van Zee is not optimistic that the link between corporate money, regulation and the practice of medicine will be broken any time soon.

“It’d be a huge missed opportunity if there’s not structural changes made in the system. But it would take an earthquake in the structure of capitalism in the United States to be able to pull that off,” he said.
The doctor does find reasons for hope. The availability of buprenorphine and other treatments has helped significant numbers of people to get a grip on their addiction, although it does not work for methamphetamines. The drug industry has paid billions of dollars to settle lawsuits by states, counties and municipalities seeking to recover the costs of dealing with the devastation caused by opioids. That money is helping to provide treatment and harm reduction.
But in the end, Van Zee said there was no escaping what the pharmaceutical industry unleashed.
“It’s gonna be a long time that people will be dealing with this. The human cost and what’s happened in our region is not easily repaired,” he said.