A woman whose treatment for a rare cancer at 15 led to early menopause has spoken of feeling "unwomanly" and "trapped in an 80-year-old’s body" as she confronted infertility and halted puberty.
Ellie Waters-Barnes, now 24, was just 14 when she received a diagnosis of Rhabdomyosarcoma, a rare soft tissue cancer, in 2015.
The initial indication of her illness was a "small, kidney bean sized lump" in her left buttock. A teenage Ms Waters-Barnes, feeling "embarrassed," delayed telling her parents for seven months.
By the time she was diagnosed, the cancer had advanced to Stage Four.
Alongside the lump, Ms Waters-Barnes experienced further symptoms including lumps in the lymph nodes in her groin, severe constipation, difficulty urinating, and a sharp pain in her left leg when engaging in her favourite hobbies of running and football.
She did not connect these disparate symptoms, believing them to be an unfortunate series of unrelated issues.
The specific location of the Rhabdomyosarcoma necessitated chemotherapy and radiotherapy focused on her pelvic area, which ultimately caused damage to her reproductive organs.
The treatment essentially halted puberty, and when her periods did not return after treatment it was confirmed that Ms Waters-Barnes was experiencing early menopause, was infertile, and that her pubescent development would not continue.
While Ms Waters-Barnes has come to terms with her infertility, she has dealt with feeling “unwomanly” and “alien” in comparison to her peers, and urges a more open conversation around the “very taboo topic” that is early menopause.
“Over time, I’ve just learned not to care,” Ms Waters-Barnes, who is now studying medicine and hopes to become an oncology doctor, told PA Real Life.
“I’ve just got to try and accept the body that I’ve been left with, and the main thing I try to do is to focus on what I can do, rather than what I can’t or what I don’t have, because there’s nothing I can do to change it.
“I’ve just got to focus on what I can do and just make the most of the body that I’ve been left with.”
Ms Waters-Barnes’ cancer symptoms all started with “a small, kidney bean sized lump that (she) discovered in (her) left butt cheek”.
“And of course, where it was, I didn’t really mention it. I was a little bit embarrassed by it,” she said.
“I didn’t actually, to be honest, at the time, think much of it. And then over the months that followed, it just kept getting bigger and bigger.
“I probably had this lump for about six, seven months before I said anything, and by the seventh month, it was basically taking up the whole butt cheek. It was pretty bad.”

Along with the lump on her buttock, Ms Waters-Barnes had lumps in her groin lymph nodes, constipation which she later learned was from the tumour pressing on her rectum, trouble urinating, and a sharp pain at the top of her left leg when she ran.
“I just thought they were separate entities, and I was just really unlucky, and that I would wake up one day and they would all be gone,” she said.
“But obviously that didn’t happen.”
Ms Waters-Barnes first noticed the lump in January 2015, but did not tell her parents until August 2015.
Over the next three weeks, she went “back and forth to the GP” who thought the lump was an abscess and tried treating it with antibiotics.
When the antibiotics did not work, Ms Waters-Barnes was sent to hospital for further checks, and ultimately learned that she had cancer.
Ms Waters-Barnes was diagnosed with Rhabdomyosarcoma – a rare type of soft tissue sarcoma that develops in the body’s voluntary muscles, such as those in the arms, legs, head, and neck, according to Macmillan – in September 2015, by which point the cancer had reached Stage Four, meaning it had spread to other parts of her body.

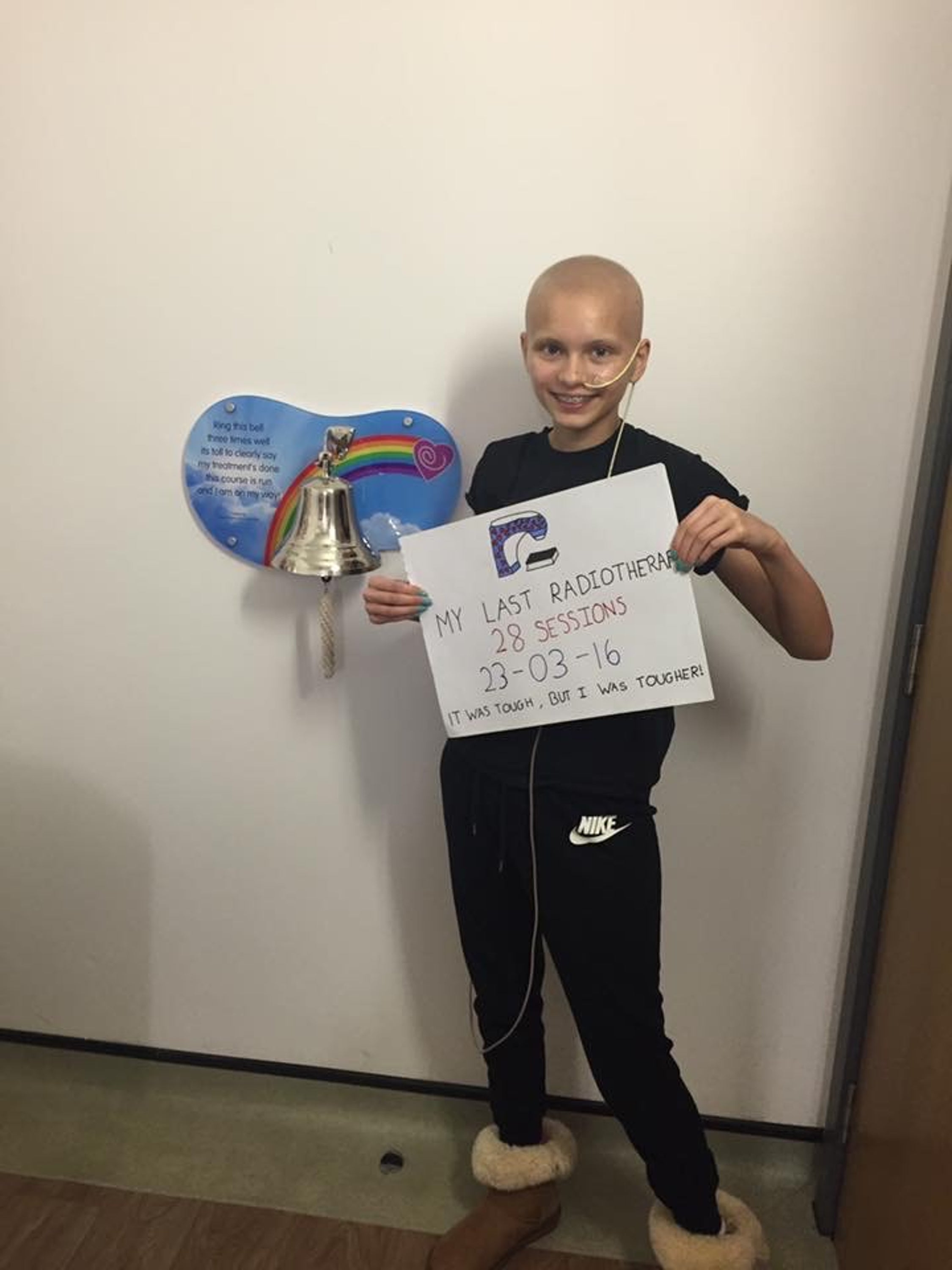
Her treatment took 18 months, and Ms Waters-Barnes said doctors “had to literally pull out all the stops for this cancer”, including nine months of intensive chemotherapy.
“It was the sort of chemotherapy that just wipes you out, like physically, mentally,” Ms Waters-Barnes said.
“My hair was gone, I couldn’t eat, had to have a feeding tube, lost lots of weight. Really bad side effects.”
Seven months into her chemotherapy, Ms Waters-Barnes began radiotherapy to her pelvis, which caused further side effects such as “terrible diarrhoea”, burning and exhaustion.
Thankfully, she did not need surgery as within four months of treatment the tumour was no longer visible on scans, but 12 months of maintenance treatment followed to ensure all remaining cancer cells were eliminated.
Finally, Ms Waters-Barnes entered remission, was able to return to school and begin her journey back to normality.
However, her future now looked a lot different to how it had before her diagnosis.
Among the long list of side effects for her chemotherapy and radiotherapy was early menopause and infertility, particularly because of the radiotherapy targeting her pelvis, though Ms Waters-Barnes said she was “in survival mode at the time” and willingly took the risk.
“I didn’t care how I was left, as long as I survived the cancer and made it out the other side, I didn’t really care at that point about the repercussions,” she said.
Ms Waters-Barnes was told that if her periods did not return within six months of her treatment ending, it would be confirmed that she was menopausal.
She was experiencing fatigue, aching, and other symptoms, though she believed these were lingering effects of the chemotherapy.
As a 15-year-old, she said she did not have much understanding of the symptoms of menopause – “I thought menopause meant no periods and maybe the occasional hot flush, and that was it” – and her mum had not yet reached that stage of her life, either.
However, Ms Waters-Barnes’ periods did not return, and she began hormone replacement therapy (HRT) – a treatment that helps alleviate menopause symptoms by replacing falling levels of oestrogen and progesterone.
“I’d not really properly gone through puberty before the treatment. With the treatment, it completely went, and then I went through menopause. There was no time to catch up, or go through puberty again. Where I left off, that was it,” Ms Waters-Barnes said.
Her arrested development made Ms Waters-Barnes lose touch with her femininity, and she found it particularly difficult when she went back to school and the other girls her age were “talking about periods, boys, hormones, and sex”.
“I felt like I was an 18-year-old trapped in an 80-year-old’s body,” she added.
“I have a bit more of a childlike body compared to my peers: My breasts never really developed, I’m still quite skinny, scrawny, not very curvy. That, alongside the infertility, and then the fact I don’t get periods, and I’ve gone through the menopause, made me feel very unwomanly.
“It affected my body image a lot, and my self worth, I felt very undesirable. I thought I’d never be able to date anyone, because I just didn’t think anyone would find me attractive in that way.”

There were also the physical symptoms: when Ms Waters-Barnes was studying for her A-Levels, she had “terrible brain fog”, was tired, aching, itching, and “could barely sit down for more than an hour because of the vaginal dryness”.
When lockdown hit in 2020 and her A-Level exams were cancelled, she began a personal research journey into early menopause, discovering that these were all recognised symptoms of menopause and that she was on too low a dose of HRT to properly combat them.
She first dealt with an NHS hormone specialist, but struggled to get the answers she needed.
Desperate, Ms Waters-Barnes paid £250 for a private menopause consultation in April 2020 and was finally prescribed a hormone replacement that worked.
“Within two weeks,” she said, “I felt like a new woman.”
While Ms Waters-Barnes finds that infertility can be “definitely a bit of a deal breaker” in relationships, she says she has come to accept it personally.
“I sort of just get on with menopause now, but I do sometimes think, when I get tired or I get brain fog or whatever: ‘If only I had normal working ovaries, maybe I would be able to perform better in my general life and my work, I wouldn’t have to remember every three days to change my patches and take hormones and all this and that’.”
Since September 2021, Ms Waters-Barnes has been studying Medicine at Keele University in Stoke-on-Trent, and hopes to qualify as a doctor in August 2026.
She is interested in specialising in oncology, using her experience to help others.

“For me, it’s just all about acceptance – accepting my situation, making sure I don’t bottle it up, talk to people about it. Then by doing stuff like this, raising awareness, it makes me feel like there’s a positive out of a bad situation. A bit of a silver lining.
“I’m able to help others, share my story and spread a bit of awareness. So that gives me a lot of solace in the situation that I’m in.”
“I think particularly early menopause is a very taboo topic that people don’t talk about,” she added.
“People are quite ashamed about it.
“I always say to people that are going through a similar situation to me: Empower yourself with knowledge. Read everything that you can about early menopause, listen to podcasts, watch documentaries, because you are your own best advocate…
“By having that knowledge, you can get access to the treatment that you need and the support that you need.
“I wish that, all those years ago, I knew a bit more.”
Claire Taylor, chief nursing officer at Macmillan Cancer Support, says: “Navigating treatment-induced menopause can be an incredibly challenging time – and many women are still going through this process feeling overwhelmed and alone.
“For anyone confronting these changes and symptoms Macmillan is here for you every step of the way providing specialist advice and support through our Macmillan Support Line, Cancer Information and Support Centres and Online Community.”
‘The exhilarating hobby that helped me overcome menopausal anxiety’
Researchers warn mutations tied to cancer risk found in 17 million Americans
CNN host Christiane Amanpour reveals cancer has returned for third time
NHS makes morning-after pill free for all women – here’s how to get it
First-ever breath test could ‘revolutionise’ care for pancreatic cancer patients
National audit reveals ‘dire state’ of treatment for stroke survivors







