“A patient wanted to buy antibiotics for a bruise. They want antibiotics even for influenza.” Indonesian pharmacists had alarming stories when researchers interviewed them about their experiences. But the story gets even more alarming: 2021 research shows that 70 percent of Indonesian pharmacies dispense antibiotics without a prescription. And many Indonesians who cannot afford appropriate health care buy prescription-only drugs, including antibiotics, in the informal sector for self-treatment. In Indonesia, licensed drug stores (which are different from pharmacies) often sell antibiotics, evading inspection by the authorities. The informal and formal sectors – licensed and unlicensed sellers, grocery stores and pharmacies – are entangled. The Indonesian distribution channels for medicines are said to be the most complicated in the world.
When prescription-only drugs are distributed without a prescription in pharmacies it seems that regulations don’t work. When they are distributed by unlicensed sellers, it shows there is a market beyond the reach of laws and regulations. Both are characteristics of a world in which low-quality drugs are prevalent. The question remains whether the problem can be solved simply by tightening regulations.
Low-quality generic drugs are a major challenge for low- and middle-income countries in two ways. First, the high availability of low-quality antimalarials and antibiotics in these countries seems to relate to demand: many consumers need these drugs. Second, the BRICS (Brazil, Russia, India, China and South Africa), an emerging group of low- and middle-income countries, need to develop their pharmaceutical business as an export industry.
A technological foundation is required to meet both these needs: satisfying local demand and succeeding as an export industry. Standards are a core element of this foundation. Pharmaceutical standards of efficacy and safety are driven by the need to protect human life. In other words, it is not possible to design pharmaceutical standards solely in terms of efficiency and convenience.
But willingness to comply with standards is not the same as achieving them. Cost is the main obstacle here. All stakeholders in a society must be motivated (incentivised) to comply with the relevant standards. It is not enough simply to strengthen laws and regulations. Medicine quality depends on a social system where all stakeholders – including approval, manufacturing, distribution and marketing entities, as well as medical practitioners and patients – receive appropriate incentives and advantages.
The public dispensary system in India is a social security system that benefits many poor people, but it is not a sound system in this respect. Officials have been caught taking bribes, and the bargaining process between suppliers and the government provides strong temptation for manufacturers to cut corners on production, making low-quality medicines to eke out greater profits.
By contrast, the public health care service in Japan is a rare example of a system designed immediately after the Second World War that continues to operate extremely well. The medical service provided under the universal health insurance system is fair, reasonably inexpensive and of good quality for all. There is ample incentive for both providers and patients to use the services. For this reason, the problem of low-quality drugs in Japan is much smaller than in other countries.
Where standards are lax and incentives to comply with them are few, there is ample room for malicious criminals. Even legitimate suppliers can find it difficult to avoid the temptation to cut costs and deviate from standards and regulations. In this way the market sees a mixture of counterfeit products made by criminals and low-quality drugs made by legitimate suppliers who fall short of specifications.
The World Health Organization (WHO) International Medical Products Anti-Counterfeiting Taskforce (IMPACT), established in 2006, defined and sought to eradicate counterfeit medicines but was silent on substandard ones. This led to significant opposition from low- and middle-income countries.
Low and middle-income countries take the view that counterfeit drugs are different from substandard drugs. But the WHO’s definition did not make this distinction clear, and internationally the two types of low-quality medicine were mixed up. High-income countries such as the United States and Germany supported IMPACT and sought to protect their intellectual property rights against emerging countries. This added to the backlash from low- and middle-income countries.
Intellectual property rights are the largest barrier to converting innovative new drugs to generic drugs, and adding them to the WHO’s model list of essential medicines. Many of the medicines in the model list are generic drugs, among which substandard drugs have been prevalent in low- and middle-income countries.
When IMPACT was established, antiretrovirals to treat HIV (AIDS) were prime candidates for inclusion in the model list from a global public health point of view, but this challenged the international rules of intellectual property rights. The conflict between the two worlds – developed and developing economies – comes clearly into view here.
IMPACT failed because from the very beginning advanced economies and international organisations drove the process, leaving the interests of a range of countries behind. The WHO needed to change course.
Tackling the proliferation of low-quality medicines is not merely a matter of enhancing pharmaceutical regulation, defining counterfeit medicines, and making technical improvements. It is also a question of international politics.
Public health policy needs to look beyond the quality of medicines to the impoverishment of those who need them. Those who risk falling into poverty if they buy good-quality medicine are forced to make a choice between low-quality medicine and no medicine at all. Paradoxically, even low-quality drugs can be a saving grace for many in the informal sector. At the same time, intellectual monopoly rights are not only the rights of one company or one industry but also a source of economic growth for some countries.
Health care is a scarce economic resource, and countries around the world are working to correct the uneven distribution of this resource. But the situation is not structurally uniform in all countries, and their external considerations are even more individualised. The gap between the ideal goals of regulation and the constraints of reality needs to be recognised.
The problem of low-quality medicines has the same source as the problem of economic inequality among people. It needs to be addressed at the same fundamental level.
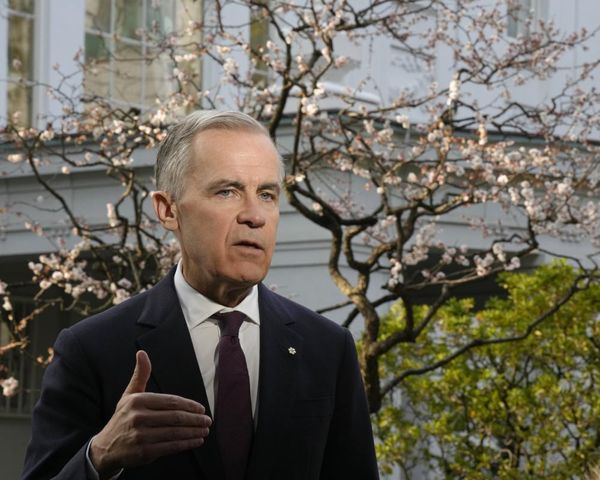
Professor Yasuhide Nakamura is a professor emeritus of Osaka University, President of Friends of WHO Japan, and a senior fellow professor of the National College of Nursing at the National Center for Global Health and Medicine in Japan.
He declares no conflict of interest in relation to this article.
Professor Nakamura thanks Dr Satoru Kimura for his excellent work in adapting material from their book, Poor Quality Pharmaceuticals in Global Public Health, to become this article. Image published under Creative Commons. Originally published under Creative Commons by 360info™.