
Tom Oxley remembers the moment his entire career trajectory turned.
It was in 2006, and an article in Nature had just been published describing the first time a brain-computer interface was successfully implanted and used in a human being.
“A patient who’d had a stroke moved a robotic limb and fed herself,” he recalls to Inverse as we sit in his office inside New York’s Brooklyn Navy Yard, overlooking the East River. “And it just opened up my mind with possibilities.”
The female patient was tetraplegic and paralyzed from the neck down. She couldn’t use her arms or legs, including her hands. But she had a rich mental life — she could think, see, hear, and speak — despite her physical disability, and she could fully process the world around her.
The ability to feed herself again was monumental on a personal level — and the way she went about it was monumental on a scientific one. The newly implanted computer in her brain, called the BrainGate sensor system, had created a direct connection between her active mind and a robotic limb. An electrical current from the brain’s cells that cue up a command — moving a thumb to text or waving a hand to say hello, or, in this case, moving a robotic limb to eat food — is captured, coded, and turned into an action via the interface. The robotic arm moved in sync with her thoughts as if it were an extension of the woman’s own body.
“I saw this as representative of an oncoming revolution in the treatment of neurological diseases,” Oxley says. And he was determined to be a part of it.

Fast forward to 2019, and Oxley, who trained as a vascular neurologist and has a doctorate in neural engineering from the University of Melbourne, is now the CEO of Synchron, a brain-computer interface company he founded in 2012. Oxley is performing his own monumental first: The implant of a Synchron-made brain-computer interface into a man with ALS.
Unlike most other brain-computer interfaces in use or in development, including the one described in the 2006 Nature paper and Elon Musk’s Neuralink (which has yet to be tested in a human), Synchron’s device doesn’t require invasive brain surgery for implantation. In fact, the entire process, as Oxley describes it during our conversation at Synchron’s office, is a two-hour-long procedure done in a catheterization lab, which is where the majority of routine cardiac stent surgeries take place. The whole process is completed in a day, and patients don’t typically have to stay in the hospital overnight. The end result is a computer sitting within the motor cortex of the brain that detects and wirelessly transmits brain activity to control a personal device like a cell phone, giving the user the ability to type a message to a loved one, for example, or order groceries, or make a doctor’s appointment, or do other quotidian tasks able-bodied people take for granted every minute of the day.
“That’s what this technology is about, opening up the possibilities of your ability to engage in the world.”
Synchron’s technology and the simplicity of the procedure, Oxley believes, will transform brain-computer interfaces as we know them. Since the 2006 breakthrough, progress on this technology has proceeded slowly. Very few companies have successfully gained approval from the Food and Drug Administration (FDA) to begin clinical trials of their devices in people. Neuralink, for instance, which is owned by Elon Musk, has only tested its devices in non-human primates, even though the company claimed back in early December that they were months away from human testing (it has yet to receive the FDA approval to do so). Others, such as BrainGate, have received FDA approval and started human testing. Still, their devices are both invasive, requiring literal brain surgery, and cumbersome, forcing users to be tethered at all times to various wires. And all of them are still in investigative clinical trials.
Some companies are working on brain-computer interface headbands, rather than unwieldy and risky implants. But these devices don’t always work; the further away you get from the brain’s inner neurons, the less powerful the device becomes. But Oxley thinks Synchron’s implant, which is essentially a stent placed at the base of the motor cortex, is the Goldilocks of brain-computer interfaces. It’s not (currently) as powerful as a device placed surgically deep into the brain, but it's minimally invasive — and it works.
Earlier this month, Synchron published the results of its initial 2019 trial. The test was performed in Melbourne, Australia, and involved four people with paralysis of their upper limbs. Synchron’s device allowed them to text, email, browse the internet, and communicate using their thoughts, demonstrating that it could translate brain signals into purposeful action.
Oxley recalls the Melbourne trial’s first participant, Graham Felstead, a man with amyotrophic lateral sclerosis, or ALS, a progressive neurodegenerative disease that affects nerve cells in the brain and spinal cord.
“With ALS, you progressively, in a very predictable fashion, lose your ability to move muscles in your body…your ability to engage in the world starts to shrink,” Oxley says. When they turned on Graham’s system, Oxley recalls, his wife came in the room, and Graham wrote out a sentence: ‘We are going to need more coffee.’
“Once you put a digital appendage in place of your hand, the sky is the limit on what you get that digital appendage to do.”
“That moment was such an inspiration for us. That’s what this technology is about, opening up the possibilities of your ability to engage in the world. We all take it for granted until you get sick,” Oxley says.
Oxley and his team at Synchron are going all in on their minimalist approach, banking on the idea that as the technology advances, they will be able to reach further and further into the brain without ever resorting to brain surgery. This will enable people with paralysis and other forms of muscular-skeletal disabilities a means to better communicate and interact with the world around them. In July 2022, following a critical green light from the FDA to begin clinical trials in humans in the United States in July of 2021, Synchron implanted one of their devices in a person at New York City’s Mount Sinai West hospital. The clinical trial, dubbed the COMMAND Study, is ongoing.
Oxley knows how far this technology could go, but the Synchron team is starting small, he says, seeking long-term gains rather than short-term wins. The device, he says, allows for an entirely novel communication stream in the brain, opening up new possibilities for neuroscience research. It could allow doctors to study poorly understood brain conditions, for example, and ultimately change how we interact with technology in the far future.
The Stentrode
At this point, brain-computer interfaces aren’t new, and Synchron’s device is far from the first or the most radical of its kind. But it has something going for it that almost no other company offers yet: Their interface does not require brain surgery.
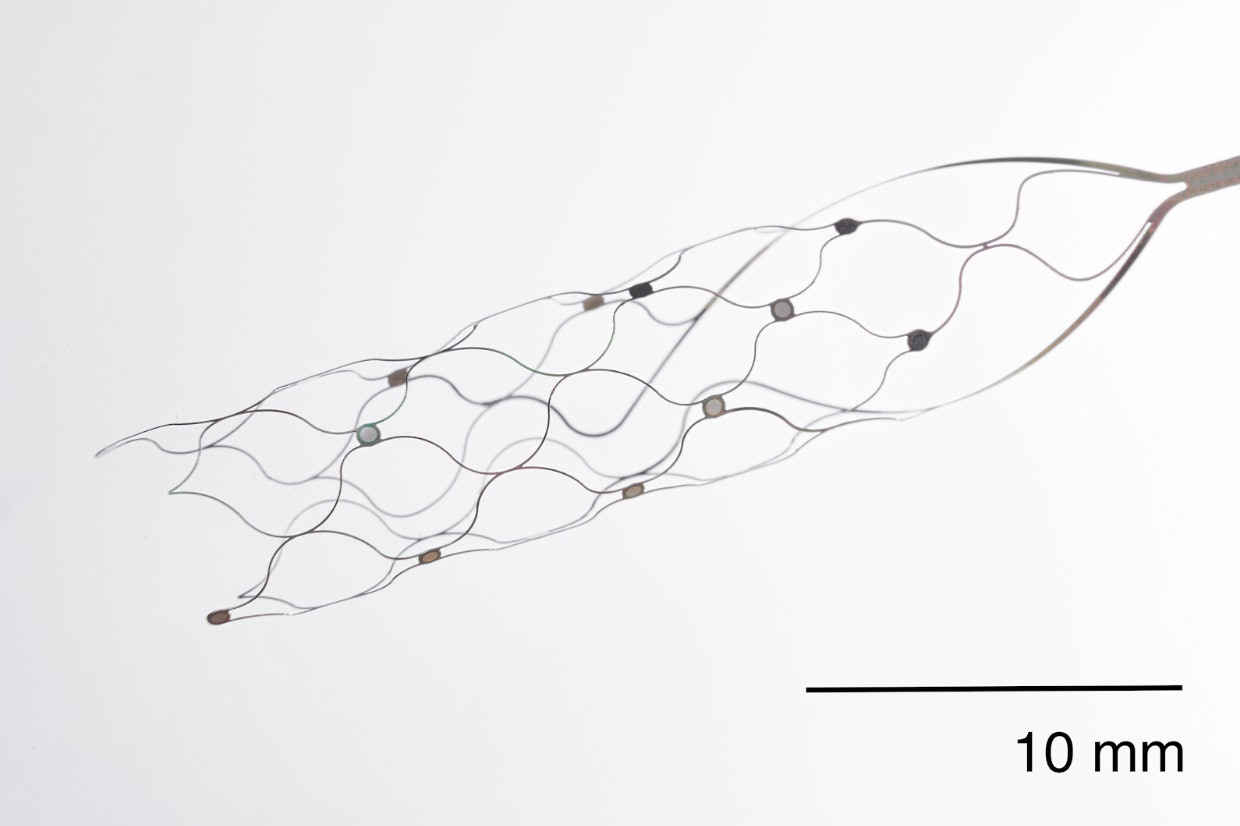
The crux of Synchron’s system is a neurovascular implant that resembles a stent (essentially a hollow mesh tube), which the company calls the “stentrode” whose structure it's more or less akin to the stents used to treat narrowed arteries in the heart or brain. In fact, the entire process, which is about two hours long, Oxley says, is similar to the procedures done to place cardiac stents, and it's performed in the same lab setup.
A neurosurgeon passes a wire into the jugular vein, through which a catheter is threaded and navigated through the superior sagittal sinus, which is a blood vessel in the brain. Once it reaches the motor cortex (which controls movement), the stentrode, which is attached to the catheter, is placed and opens up like a flower, says Oxley, forming a scaffold around the inner wall of the blood vessel. A wire is then threaded through to a device that sits just under the skin in the person’s chest.
The device is then connected to an external system outside the body and can connect to other devices via Bluetooth. The stentrode collects any signal from the motor cortex and sends it, via the wiring, to the decoder, which, using a machine learning algorithm, converts the signals into commands, such as say, typing to text that you’d like some more coffee.
The stentrode is designed to be permanent, but Oxley acknowledges that the technology will likely advance — making replacements and upgrades more likely.
“There is always the likely future that there is going to be newer and smaller devices. So you can’t remove the stent, but you can put in new stents.” The electronics that are separate from the stent can be upgraded, too, he says.
Unlike the invasive brain surgery required to implant other interfaces, Synchron’s procedure allows people to go home the same day. Additionally, the procedure itself mimics one that most neurosurgeons perform on a routine basis.
“There’s a reason why, since 2006, it’s been proven that [BCIs are] really effective, but there’s still no commercial product,” says Oxley. But the growing field of neuro intervention, where stents are placed into the brain, is where Oxley sees endless possibilities: “They can get to really deep regions within the brain now in tiny blood vessels.”
“We start with a certain blood vessel in a certain part of the brain that will treat a certain group of people, but the technology is going to continue to mature and improve,” he adds.
Synchron’s long game

Oxley’s focus now is to continue the COMMAND study, his ongoing clinical trial in the U.S. So far, Synchron has implanted three patients in the U.S. The company says it will implant a total of six devices in people by June 2024. After that, the company plans to conduct another trial to further prove safety and effectiveness before its device — which it calls the Synchron Switch — can be eligible for Medicare and insurance coverage.
Ultimately, Oxley’s goal is to perfect Synchron’s device, and he asserts making it work primarily for people with severe paralysis.
“Paralysis is a very big problem and is caused by a range of conditions from stroke to spinal cord injury and even Multiple Sclerosis. You lose your ability to control your body, but your brain is still working,” he says. “The starting point for us is to help the most severely impaired people regain control of personal digital devices to improve their ability to function independently.”
Sychron’s biggest obstacle is, paradoxically, also a part of its success: Because it chose the blood vessel route, the device is more limited than some of its competitors, as they are directly implanted deep in the brain. Within our cortex, there lies a large mass of inter-tangled neurons. If you stick needles directly there, as Synchron’s competitors like Neuralink and BrainGate are trying to do or have done, you can record information from more neurons at a time.
“The downside of penetrating electrodes as opposed to surface electrodes is that we don’t really know about proving safety over a long period,” Oxley says.
“What ability are you expecting or do you want?”
Synchron, by contrast, targets blood vessels that run along the brain's surface. Its device is safer and less invasive, but it is also, perhaps, slightly less effective.
Oxley isn’t worried that his device is currently less targeted and less precise than his competitors. Because blood vessels are like branches of a tree, they split into smaller and smaller extensions and continue to inch further into the brain. “We started with a big blood vessel with a certain amount of access, and we are building a pipeline of miniature technologies,” Oxley says. “There is going to be increasing access to more and more data from the brain to increase the ability of the system to work. So no, we’re not there yet, but we have a path to get there.”
What’s next?

When asked about the future of brain-computer interfaces, Oxley says it's hard to predict, because the way we interact with technology, including screens and computers, is changing so fast. But what he is certain of is that this technology will help people with severe paralysis.
“It’s going to initially start in the motor cortex, which is the domain of movement. The things that we learn from interacting with the brain cells in that region are going to be the same for the control of other domains of function in the brain. So, once we’ve gotten a product that can interact with the motor cortex, we will go and think about other regions of the brain,” Oxley says.
Beyond that, things start to blur.
Mainly, we don’t yet understand all the inner workings of the human brain and its various processes to know how brain-computer interfaces will change and grow. But Oxley says that using them will be a big part of that. If the BCI represents the brain’s intent, it can do it in many ways. “Once you put a digital appendage in place of your hand, the sky is the limit on what you get that digital appendage to do,” he says.

It also opens up the possibility of studying diseases outside of muscular-skeletal ones. He likens BCIs to a two-way radio in the brain.
“The concept of this two-way information flow in the brain is interesting from an emotional perspective, from a memory perspective, from a hearing perspective. You start to engage in downflow within the brain in those domains, which can open up avenues of treatment for a range of conditions.”
If the technology advances far enough, will these devices become ubiquitous? Oxley sees a similar, perhaps even blurrier, scene.
“When I speak to people, they say I wouldn’t use it unless I lost my ability to do something,” he says. But as the world advances, the question becomes: “What ability are you expecting or do you want?”
Photographs by Hannah Whitaker
THE FUTURE OF YOU explores the tantalizing advancements in personal health, from a future without periods to computers in our brains. Read the rest of the stories here.
Editor’s note: This story has been updated with the correct name of the ongoing U.S.-based clinical trial of Synchron’s device — the COMMAND Study. The SWITCH Study was conducted in Australia. We are glad to correct the error.
.jpg?w=600)






