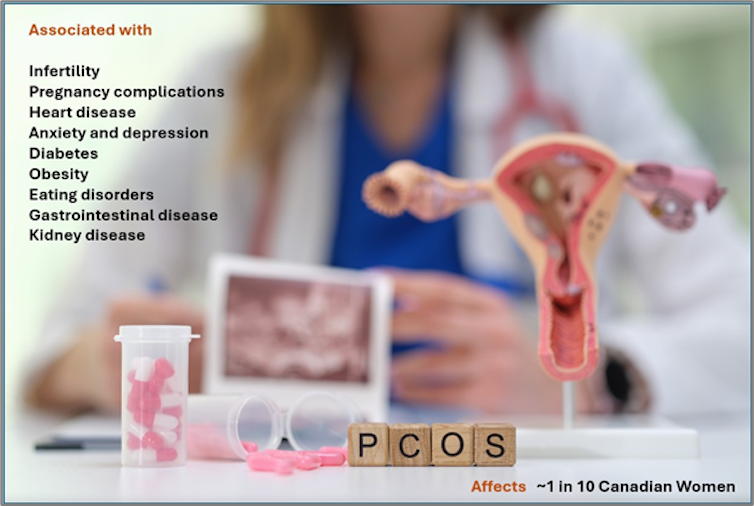
Polycystic Ovary Syndrome (PCOS) is a hormonal imbalance that affects ovaries, periods and fertility in about one in 10 Canadian women. Different from ovarian cysts, PCOS is associated with infertility, pregnancy complications, heart disease and a general decreased quality of life, and yet fewer than half of those affected even know they have it.
This under-recognition and under-diagnosis is a significant problem, because a recent Canadian study suggests these women are 20 to 40 per cent more likely to experience negative health outcomes during their lifetime than the general population, including hypertension (high blood pressure), kidney disease, gastrointestinal disease, eating disorders, depression and anxiety.
Heart disease risk
The Canadian researchers also found obesity, dyslipidemia (abnormal levels of fat in your blood) and Type 2 diabetes to be two to three times more common for women with PCOS. And most importantly, cardiovascular disease, which causes heart failure and stroke, was not only 30 to 50 per cent more likely, but occurred three to four years earlier than average in women with PCOS.
Cardiovascular disease is the leading cause of death worldwide, so when PCOS symptoms are missed and untreated, women’s health is at risk.
High cost
There is undoubtedly a personal cost to individual women, both physically and mentally, and living with PCOS can be a significant financial, health-care and work-life burden for many women, too, which may disproportionately affect those in lower socioeconomic groups.
These experiences are further compounded by a system failure to properly diagnose and manage their symptoms. Women report doctors ignoring or dismissing their concerns, not believing them and struggling to make a diagnosis. In fact, a large international survey reported it can take several months, and even several years, before women are diagnosed.
Common PCOS symptoms
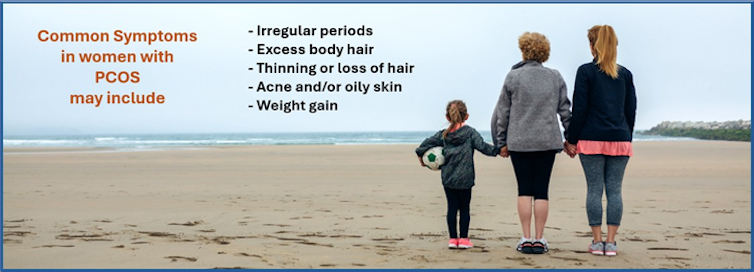
PCOS symptoms can vary between different women, but it is important to discuss the possibility of PCOS with your doctor, because careful management and/or treatment can help protect against developing more serious related health issues. Common symptoms include:
- Irregular periods
- Excess body hair, called hirsutism (usually darker hair on the face, arms, chest or abdomen)
- Thinning or loss of hair (like excess body hair, this is caused by high levels of male hormones, or androgens)
- Acne and/or oily skin
- Weight gain
Managing and treating PCOS
Despite PCOS first being diagnosed almost a century ago, there is no single test to confirm whether a woman has it, and there is no cure. If your doctor suspects you may have PCOS, they may order blood work to check your hormone levels and an ultrasound to check your ovaries.
Unlike ovarian cysts, which are fluid-filled sacs that develop on or inside an ovary and can be painful, polycystic ovaries are enlarged, with multiple follicles that can be seen on ultrasound.
If PCOS is diagnosed, further testing for cholesterol and glucose levels is likely in order to manage heart disease and diabetes risk.
Researchers also suggest ways women with PCOS can help manage their condition, which include:
- Eating a healthy diet
- Exercising regularly (including strength training with weights)
- Sleeping for at least seven hours each night
- Reducing stress (work-life balance; deep breathing exercises)
- Relaxing in your favourite way (such as yoga, mindfulness and meditation, hobbies)
PCOS research underway
Despite the current problems, improvement is possible, and there have been sustained efforts in recent years — all over the world — to advocate for women with this condition and invest in PCOS research.
In 2023, an International PCOS Guideline, led from Australia, was published. It recommends an individualized approach to PCOS treatment, including lifestyle modifications (for example, healthy eating and exercising), medical management to treat symptoms and regular checkups to provide support and screen for related complications.
In Canada, the province of Alberta recently launched a much-needed clinical pathway to recognize, treat and advocate for PCOS that could be adopted more widely.
At the University of Calgary, Dr. Jamie Benham, one of the authors of this story, leads EMBRACE (Endocrine, Metabolic and Reproductive Advancements), a new women’s health research lab where a team of clinical researchers is focusing on reproductive disorders across the whole of a woman’s life system, including PCOS and gestational diabetes.
This work, supporting patients’ PCOS care, includes a current online needs-assessment survey, and focus groups beginning later this year, to inform the development of a co-designed patient tool to support PCOS management.
Patient engagement
With such a huge demand for answers, the EMBRACE team works closely with a PCOS Patient Advisory Council, chaired by Robyn Vettese, another author of this story, to uncover complex connections between hormones and health, promote screening, find solutions and provide answers. Importantly, the lab’s research questions come directly from clinic patients, and the answers the lab finds go back to those patients and are then shared more widely.
Other recent PCOS advocacy events include Dr. Benham’s presentation at the inaugural Sex, Gender and Women’s Health Research Hub’s Women’s Health Symposium event in Calgary, and her interview with the Libin Cardiovascular Institute.
PCOS awareness
Another exciting research program in Alberta is PCOS Together. Researchers with this group are working to establish methods that will detect early disease risk in all women with PCOS, as well as clinical interventions that will help prevent disease in high-risk women.
Similar organizations exist in the United Kingdom and Australia, including Verity PCOS, a volunteer-based charity, and Ask PCOS, a researcher- and clinician-led organization. Both organizations provide a wealth of information online.
This is a critical (albeit often overlooked) area of women’s health that needs greater awareness and attention so that we can improve and save women’s lives.
Jamie Benham receives funding from the M.S.I. Foundation, Diabetes Canada, and the Canadian Institutes of Health Research.
Robyn Vettese receives funding from the Canadian Institutes of Health Research.
Pauline McDonagh Hull does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
This article was originally published on The Conversation. Read the original article.







