
A new blood test will be offered to lung cancer patients in a move that NHSEngland says will benefit about 15,000 people each year.
The test, known as a liquid biopsy, is designed to speed up access to targeted treatments and avoid the need for unnecessary biopsies, officials have announced.
It works by analysing a blood sample to look for tiny fragments of tumour DNA and detect mutations which would allow patients to access therapies tailored to the genetic profile of their disease much faster.
The test will also be used to check breast cancer patients for a wider range of genetic variants to see if they are eligible for targeted treatments, with plans to explore how it could be used for more forms of cancer.
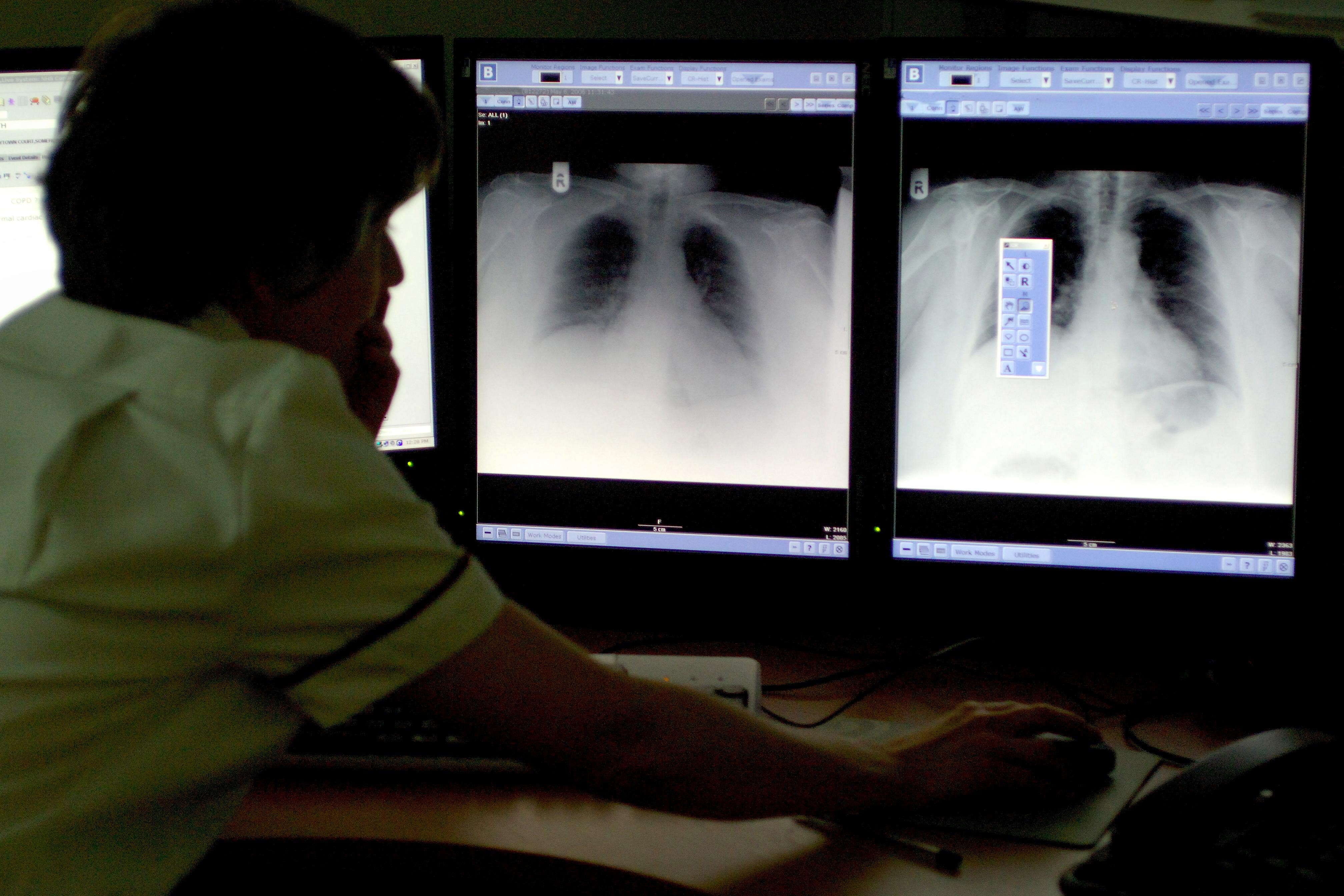
Lung cancer is usually diagnosed with a combination of scans and biopsies, during which specialists take a small sample of lung tissue to examine under a microscope.
While tissue samples can be sent for genomic testing, which shows genetic mutations linked to cancer development, liquid biopsies mean patients get results faster.
About 10,000 people with non-small cell lung cancer – the most common type – have already had a liquid biopsy as part of an NHS pilot involving 176 hospitals. The wider world-first rollout is expected to benefit 15,000 patients every year.
Professor Peter Johnson, NHS national clinical director for cancer, said liquid biopsies are “leading us into a new era of personalised cancer care, and it’s fantastic that we are now able to expand the use of this revolutionary test on the NHS to help tailor treatment for thousands of patients across the country.”
The pilot scheme showed that patients who had a liquid biopsy were able to make decisions on treatment an average of 16 days earlier than those who had tissue biopsies.
Independent analysis of the pilot estimated the test could save the health service up to £11 million a year in lung cancer care.
The NHS is exploring how it could be used for other cancers, including pancreatic and gallbladder cancer, officials said.

The health service will also test patients with advanced breast cancer who have not responded to treatments for a wider range of genetic variants to see if they are eligible for targeted treatments. It is expected that 5,000 women a year will benefit from the move.
Prof Johnson added: “Cutting-edge genomic testing is helping us deliver more targeted and kinder care for patients, enabling some to avoid more intensive treatments such as further chemotherapy, which can have a huge impact.
“We are already seeing the difference this test can make in lung and breast cancer, and we hope to roll it out for patients with other forms of cancer in the near future.
“As research progresses, it’s exciting that this approach has the potential to help us ‘scan’ the body in a single blood test to see where and how cancer may be developing and target it with speed and precision to help save more lives.”

Health Secretary Wes Streeting said the new testing will “give thousands of people peace of mind”.
Professor Dame Sue Hill, chief scientific officer for England, said: “This represents a real step-change in care for eligible lung and breast cancer patients on the NHS.
“This testing is transforming care and helping clinicians match patients earlier, especially when cancer tissue may not be available with potentially life-extending targeted therapies rapidly and with greater precision.
“This test is a great example of the NHS harnessing the power of genomic technological advances to enable the latest groundbreaking treatment to be delivered to patients.”
Symptoms of lung cancer
NHS
The main symptoms of lung cancer include:
- a cough that does not go away after 3 weeks
- a long-standing cough that gets worse
- chest infections that keep coming back
- coughing up blood
- an ache or pain when breathing or coughing
- persistent breathlessness
- persistent tiredness or lack of energy
- loss of appetite or unexplained weight loss
Less common symptoms of lung cancer include:
- changes in the appearance of your fingers, such as becoming more curved or their ends becoming larger (this is known as finger clubbing)
- difficulty swallowing (dysphagia) or pain when swallowing
- wheezing
- a hoarse voice
- swelling of your face or neck
- persistent chest or shoulder pain
Rebeca Proctor, 41, from Carlisle, was diagnosed with stage 4 non-small cell lung cancer in January.
The results from a liquid biopsy showed she had an ALK genetic mutation, meaning she could start the targeted treatment, brigatinib.
A tissue biopsy confirmed the mutation around 10 days after her liquid biopsy results.
Ms Proctor said: “When I found out I had stage 4 cancer it felt like I’d been punched in the gut. I was scared – I just thought about my children, and if I would get to see my little girl start nursery, and how I would explain my diagnosis to my children. It was just heart-breaking to think about.
“But the medication has given me my life back and my kids have got their mum back. I’m taking it day-by-day and for now the treatment is doing what it’s meant to be doing and shrinking the tumour, and I’ve got my energy back.
“I know I’m not going to be cured but I’ve come to terms with my diagnosis and the pills are stopping my cancer cells from spreading. We’ll keep fighting this and dealing with what’s been thrown at us.”
Parent intuition ‘can predict serious illness’ in children – study
NHS to roll out ‘revolutionary’ blood test for lung cancer
Planning rules eased for electric vehicle chargers
Common herbal supplements could be linked to deadly liver damage
Here are the 10 riskiest foods to eat in the US right now
This common over-the-counter drug could be linked to dementia







