Editor’s Note: The Atlantic is making vital coverage of the coronavirus available to all readers. Find the collection here.
In last week’s update, we wrote that the United States had reported the worst weekly case, hospitalization, and death numbers of the pandemic. At the time, it wasn’t clear what proportion of the case and death increases were related to postholiday reporting backlogs. This week brings some clarity: The backlogs appear to be largely behind us, and the underlying trends are moving in the right direction for most of the country. Even for the states experiencing the worst outbreaks, we are seeing early indications that the rates of cases, hospitalizations, and deaths are easing, though some areas are still reporting dangerously high case and hospitalization levels and wrenching death rates.
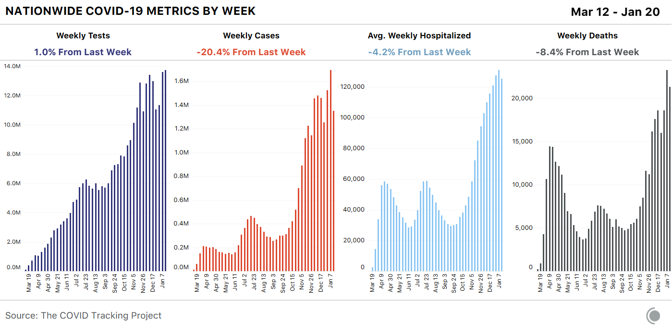
Weekly new cases for the seven-day period beginning Thursday, January 14 were down 20 percent, the lowest number of new cases we’ve seen for a non-holiday week since mid-November. As important, after 16 straight weeks of increases, average weekly hospitalizations dropped 4 percent this week—a modest improvement, but a good sign. Reported tests reached a new weekly high, edging out last week by 1 percent—though the high test numbers this week probably reflect the fact that the testing backlog is still catching up.
[Read: The most reliable pandemic number keeps getting worse]
States reported 21,301 deaths this week, the second-highest number of deaths of the pandemic to date. Yesterday, states reported 4,409 COVID-19 deaths, the highest single-day number of deaths on record. For comparison, in the week of September 24, 2020, states reported fewer than 5,000 deaths for the entire week.
Because of the way states report data for nursing homes, assisted-living facilities, and other long-term-care facilities, our figures for COVID-19 in these facilities refer to the week beginning January 8. These numbers remain very alarming: For the second week in a row, LTC facilities reported the highest death toll since we started gathering long-term-care data last May—more than 7,000 residents and staff. The number of known deaths reported this week may include backlogged figures from the winter holidays, and they also got a boost from a change in Iowa’s death reporting that increased that state’s reported figure.
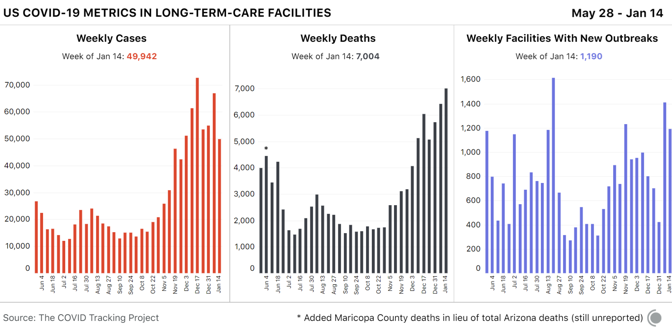
There is also tentative good news from long-term-care facilities: The number of new cases was down by about 15,000 this week. It remains unclear whether case data have fully normalized from the reporting delays associated with the holidays, but next week’s data should confirm whether this case drop indicates a real improvement in the situation in long-term-care facilities.
Regional hospitalization and case data
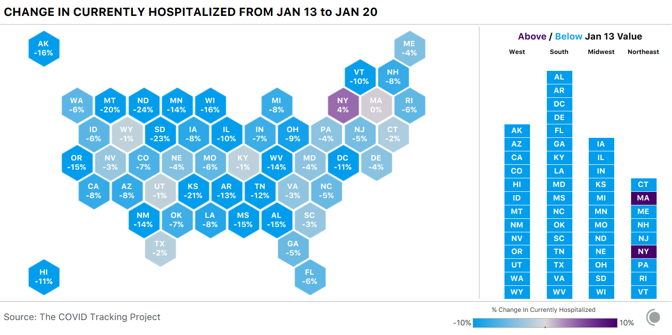
A closer look at current COVID-19 hospitalizations offers good news for most U.S. regions. Hospitalizations remain very high but are declining modestly across the South and the West and continuing their substantial declines in the Midwest. In the Northeast, hospitalizations have plateaued.
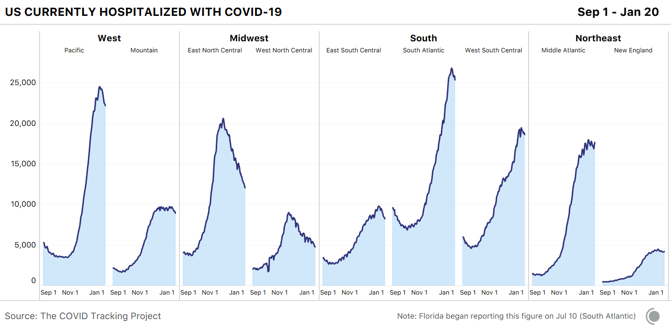
At the state level, hospitalization data remain encouraging: Hospitalizations are declining or flat in every state but New York.
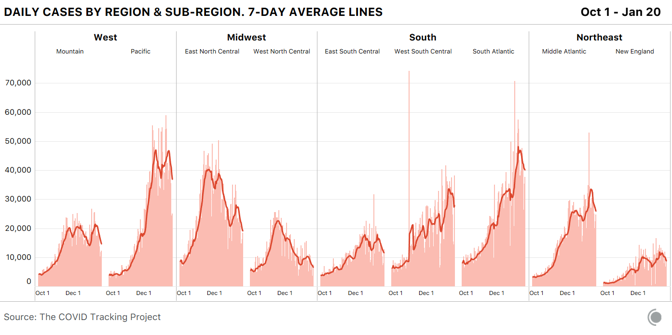
Cases, too, are falling in every region. In the Midwest’s “West North Central” division—which includes many of the states that had the worst per capita outbreaks late last fall—cases have very nearly returned to the levels reported at the beginning of October 2020.
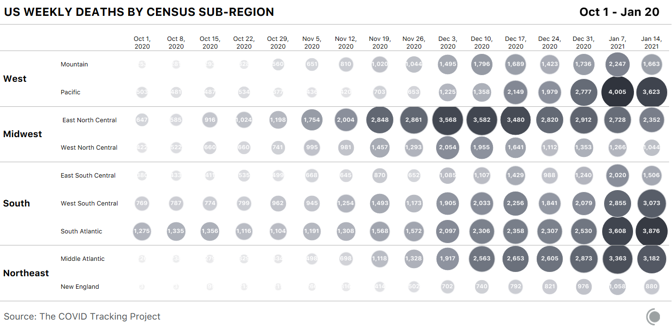
A breakdown of weekly reported COVID-19 deaths by census regions and subregional divisions shows that although deaths are falling modestly across the country, they remain painfully high in most regions.
States we’re watching
Case and hospitalization declines are unquestionably good news. At the same time, in the country’s worst hot spots, states are still reporting very high numbers.
Arizona’s case count has fallen from last week, but per capita, the state’s case numbers remain the highest in the country at a seven-day average of 958 per million. The state is now nearly tied with South Carolina, where cases are rising rapidly. In Yuma County, Arizona, home to many of the state’s seasonal laborers, the Associated Press reports that the county has a positivity rate of 20 percent, compared with 14 percent for the state as a whole, and county public-health authorities said last week that they had run out of vaccines.
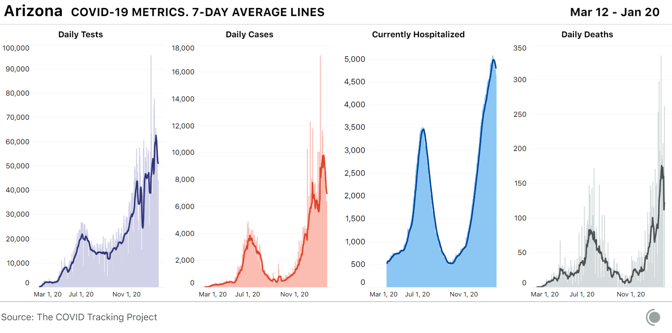
Hospitalizations lag behind cases, and Arizona’s per capita hospitalizations remain by far the highest in the country. Arizona’s hospitals are under severe strain, with 92 percent of all ICU and inpatient beds occupied as of Wednesday, accompanied by a surge in pediatric COVID-19 hospitalizations. Nursing homes are also experiencing an increasing number of cases and deaths, and Fox 10 Phoenix reports that 40 percent of Arizona COVID-19 deaths have come from nursing facilities. Despite this, delays in the distribution of vaccines mean that many facilities (and patients) are still waiting for the first doses.
[Read: A vaccine for kids is coming, slowly]
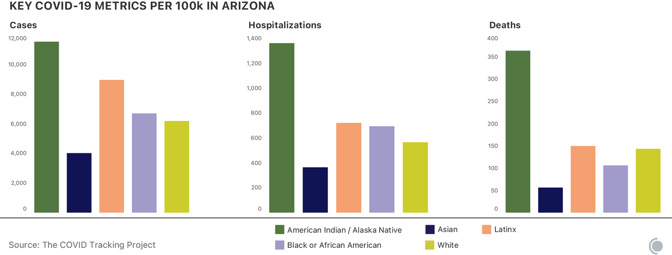
The disparity in COVID-19 outcomes for Indigenous people in Arizona has been pronounced throughout the pandemic. At least one in nine people identified as “American Indians or Alaska Natives” has tested positive for COVID-19 in the state, while one in 16 white residents has. Indigenous people in Arizona are more than twice as likely to have been hospitalized with COVID-19 as their white neighbors, and more than 2.5 times as likely to have died.
California, which reported the third-highest number of new cases per capita this week, is finally seeing the number of new cases reported each day begin to decline. Even the state’s Southern California epicenter is seeing modest but important improvements: Following weeks of record-breaking cases and hospitalizations in Los Angeles County, the number of new cases per day is down 17.6 percent from two weeks ago, and hospitalizations are down 10 percent over that same time period, according to data from the Los Angeles Times. County officials warn that the virus is still surging in the area, and that hospitalizations remain at dangerously high levels, with ICU numbers remaining nearly unchanged over the past two weeks.
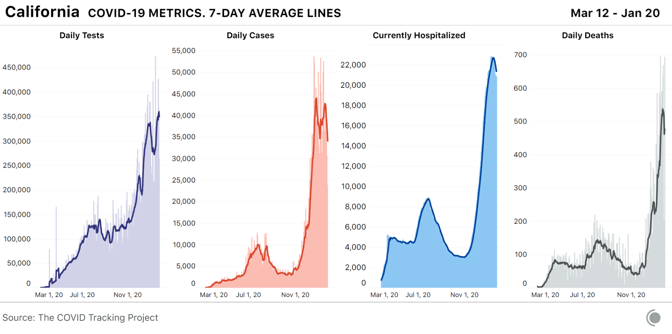
On Wednesday, the state surpassed 3 million total cases to date, meaning that one in 13 Californians has tested positive since the start of the pandemic.
As we’ve seen over the entire course of the pandemic, rising cases lead to rising deaths. The massive number of cases in Southern California over the past month has resulted in a wrenching death toll: The state reported 3,331 COVID-19 deaths in the past seven days alone. In Los Angeles County, air-quality rules limiting the number of cremations each day have been suspended to allow crematoriums to clear a backlog of bodies at hospitals and funeral homes.
In California, people identified as “Native Hawaiian and other Pacific Islander” are being disproportionately harmed by COVID-19. Although they make up a small part of the population, Native Hawaiians or other Pacific Islanders are three times as likely to have tested positive for COVID-19, and 1.8 times as likely to have died, as their white neighbors. Black people in California are 1.4 times as likely to have tested positive for, or died of, COVID-19 as white people in the state. Latino Californians, the largest single racial or ethnic group in the state, are 2.6 times as likely to have tested positive and 1.4 times as likely to have died as white residents.
Alabama, which had the second-highest number of COVID-19 hospitalizations per capita last week, has now reported its highest ever number of weekly COVID-19 deaths. In a gruesome echo of Southern California’s outbreak, Alabama crematoriums are running “around the clock” to manage the increased demand. According to the CDC, Alabama also has the lowest COVID-19 vaccination rate of any state, although the Alabama Department of Public Health disputes the CDC’s numbers.
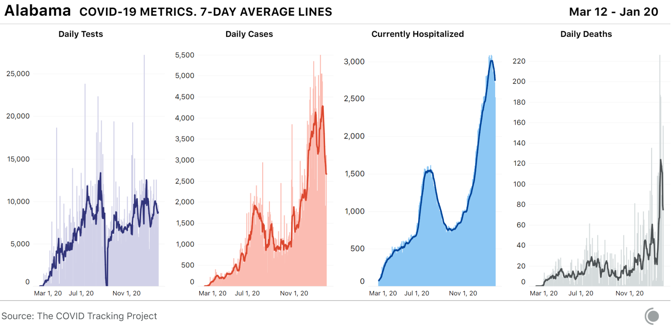
The Black population of Alabama is being hit hardest by the state’s outbreak. Over the past two months, the number of cases per capita for Black people has increased more quickly than for other groups. For the 57 percent of Alabama cases where race is reported, Black people are more likely than anyone else in Alabama to have tested positive for COVID-19, and they are the most likely to have died.
[Read: The virus is showing Black people what they knew all along]
Adjusted for population, Nevada had the second-highest number of people in the hospital with COVID-19 this week. It also reported its highest ever single-day number of deaths on Wednesday, most of which were reported in Clark County, where Las Vegas is located. Originally intended to be lifted this week, the state’s COVID-19 restrictions have been re-extended until February 15. On January 15, the Las Vegas Review Journal reported that a total of 40 prisoners in the state had died due to COVID-19, a number that is more than four times higher than the state’s eight cumulative deaths among prisoners as of January 7.
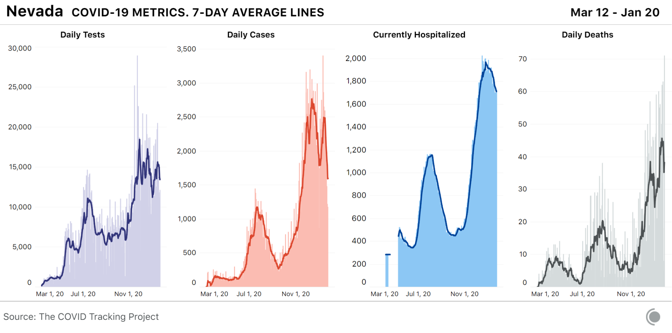
Throughout the pandemic, Latino people in Nevada have been more likely to experience COVID-19 than their white neighbors. One in nine Latino people has tested positive for COVID-19, compared with one in 15 white people in Nevada.
We are frequently asked for data on known variants of SARS-CoV-2, the virus that causes COVID-19. At present, very little data on the spread of variants exist in the United States, and we need much more genomic-sequencing data to understand the degree to which the virus is changing, and where variants are appearing. Unfortunately, the U.S. currently ranks 43rd in the world for percentage of cases sequenced. By contrast, the United Kingdom, where the widespread B.1.1.7 variant was first identified, is ranked eighth in the world. Earlier this month, the director of the U.S. Office of Advanced Molecular Detection at the CDC’s National Center for Emerging and Zoonotic Infectious Diseases announced a plan to more than double the number of samples sequenced, from approximately 3,000 samples a day to about 6,500. The U.S. is currently reporting more than 200,000 new cases of COVID-19 each day. A state-run lab in Colorado was the first in the U.S. to identify a B.1.1.7-variant case this year and it is now routinely screening all samples submitted to the lab for this mutation. The Colorado Department of Public Health and Environment has also added variant case counts to their COVID-19 dashboards. To date, most states lack the resources to add genomic surveillance to their ongoing COVID-19 workload.







