Hunter residents on marginal incomes may have to travel to Western Sydney to find a bulk-billing GP, a prominent doctor says.
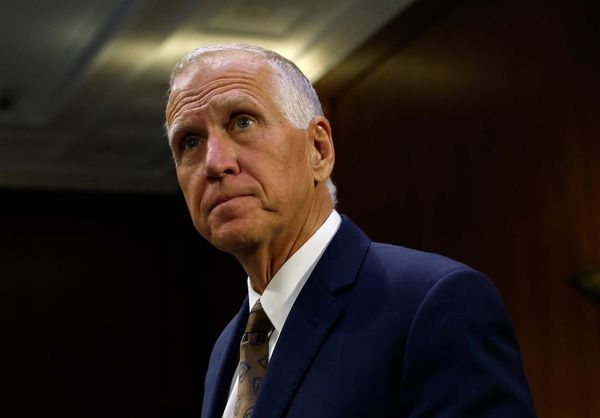
Dr Lee Fong, a Newcastle-based GP, said numerous bulk-billing doctors in Western Sydney were listed on the HotDoc website - along with two on the Central Coast.
His comments follow concerns about people in the Hunter not being able to afford to see a GP.
"A patient could potentially travel once to visit a GP [in Western Sydney] to establish a relationship," Dr Fong said.
This would then enable "bulk-billed telehealth consultations for the next 12 months".
"This is very far from an ideal solution, but for some perhaps it is the only realistic one at this time."
He said access to healthcare would be "increasingly determined by the out-of-pocket private fees you can afford to pay".
Dr Fong, the Hunter General Practitioners Association secretary, said Medicare had been intended to guarantee "access to a wide range of health and hospital services at low or no cost".
The cost for a standard GP consultation is about $70 to $90 in the Hunter, with a Medicare rebate of about $40. As such, people are faced with an out-of-pocket gap fee of up to $50 to see a doctor.
In the May federal budget, the Albanese government announced $5.7 billion over five years to "strengthen Medicare and make it cheaper and easier to see a doctor".
This included new incentives for GPs to bulk bill patients aged under 16, pensioners and concession card holders.
GPs said this wasn't enough to resolve the difficulty most people have in finding a doctor who bulk-bills.
"Unfortunately we've gotten to a point where, certainly for access to general practice, the system is broken," Dr Fong said.
"The reasons for this are complex, but include a population that is living longer with chronic diseases."
Other factors were increasing social isolation and a system designed and funded "for more acute rather than chronic presentations".
He said the system needed "reforms that better suit our nation".
"There are reforms on the way, but these will not happen rapidly and don't fully address the underlying issues," he said.
He predicted more people with "marginal incomes" will find it "increasingly difficult to access basic healthcare".
As well as broad reforms, he said "more agile local solutions" were urgently needed for "those being left behind".
The Newcastle Herald recently reported that Mitchell Patterson and Emma Haining were turned away from the Mater's psychiatric emergency centre on the same night.
Both were taken to the Mater by ambulance in deep distress and suffering from suicidal thoughts.
They had been unable to see a GP to discuss their condition.
"We need people like Mitchell and Emma to talk to their local state and federal members to highlight how bad the problem is," Dr Fong said.
"And then we need the health system - hospitals, general practice/primary care - to come together with all three levels of government to come up with and fund solutions."
Dr Fong said there were "lots of possibilities".
This included "leveraging the Medicare safety net" or "establishing targeted services to specific populations".
"For anything to happen, we need all the players to come together and agree on a way forward."
Lifeline 13 11 14.