Doctors started writing their wills and making sure their life insurance was up to date when the pandemic began in 2020 because they understood “what was coming”, the UK Covid inquiry heard on Thursday.
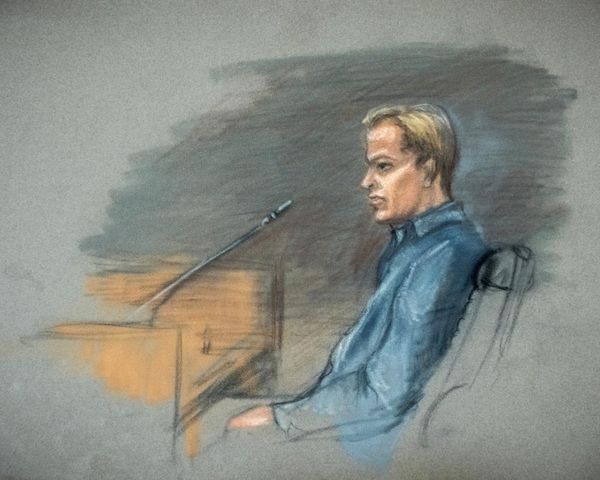
Giving evidence to the inquiry, Prof Philip Banfield, from the British Medical Association, said: “We had no doubt that we were facing something that was completely unprecedented.”
Banfield said that after 2022, the medical profession needed “to undergo a kind of grief debrief”, adding: “It was very clear that the profession was traumatised not only from within itself but from what didn’t seem happening for its patients.”
Banfield criticised the government’s actions during the pandemic on a number of grounds, including:
Their failure to include an official, strong, independent public health presence on the public stage.
Their slowness in introducing face masks. “Policies like face masks were based on a political narrative rather than a public health narrative: specifically economic and other factors that lay outside public health,” he said.
The decision to shift away from contact-tracing on 12 March 2020, which failed to control the population for a further 11 days.
The consequences of “eat out to help out”, which drove up new Covid-19 infections by between 8% and 17%.
The “chopping and changing” of the three-tier structure, which limited people to restrictions including staying overnight only with those in one’s household or support bubble and working from home where possible.
Banfield also flagged the lack of PPE. “We had stories very early on about not being able to have PPE,” he said. “There were a lack of aprons and visors. A number of us had to have our local schools 3D printing visors for us. A number of people had to source masks themselves.”
Later in the afternoon, James Nazroo, a professor of sociology at the University of Manchester and co-director of the Manchester Institute for Collaborative Research on Ageing, said that the government should have been clear what the impact of the pandemic on residents in care home and long-term care facilities would be because of a paper published in 2017.
This paper, co-written by Jonathan Van-Tam, deputy chief medical officer during the pandemic, warned of the dangers of a pandemic on those in long-term care.
The paper warned the impact could be “explosive” – with care home workers very likely to spread the disease if they were moving between homes while being asymptomatic, or if they had symptoms but couldn’t afford to take sick leave because of economic pressures.
At the time that this article was published, Van-Tam was a professor of public health at Nottingham University. The paper presented evidence that “long-term care facilities present a population very susceptible to the acquisition and spread of infectious diseases, and for whom the consequences of infection may be serious”.
Nursing home residents, the paper found, were at greatest risk due to residents’ overall frailty, close-quarter living arrangements, shared caregivers, and opportunities for introduction.
The paper was, Nazroo agreed, “prophetic”, adding that it . “explains the risks very clearly”.
“First of all, he was flagging the basic vulnerability of nursing and care home occupants to a flu-like virus on account of their own frailty and their close living arrangements.”
The paper noted that the prevention and control of influenza in these facilities required a multifaceted approach. Nazroo agreed, saying: “Vaccination and antiviral policies form an important part of this but strong managerial leadership, outbreak planning, and a well-trained, educated and engaged workforce are pivotal to the successful implementation of infection prevention control policies.”