Brain cells “clogged” with fat could be hidden drivers of Alzheimer’s disease, according to a new study that shifts focus away from protein plaques and tangles thought to be the main contributors behind the condition.
For decades sticky misfolded protein plaques and tangles – abnormal accumulations of specific proteins in the brain – have been the main suspects thought to cause Alzheimer’s disease, with most drugs developed against the condition targeting these molecules.
It was long thought that fat in the brain did not play any role in such neurodegenerative diseases.
Now, a new study, published in the journal Immunity, shows that excess fat in the brain’s resident immune cells, such as the microglia, could be impairing them and contributing to Alzheimer’s.
"In our view, directly targeting plaques or tangles will not solve the problem; we need to restore the function of immune cells in the brain," said Gaurav Chopra, an author of the study from Purdue University.
“We're finding that reducing accumulation of fat in the diseased brain is the key, as accumulated fat makes it harder for the immune system to do its job and maintain balance,” Dr Chopra said.
Microglia are known to clear out debris, including misfolded proteins such as amyloid beta and tau, by absorbing and breaking them down.
Researchers hope new treatments for neurodegenerative diseases like Alzheimer’s and Parkinson’s diseases could be developed by targeting these fat accumulation pathways and restoring the ability of the brain’s immune cells to fight disease and keep tissues in balance.
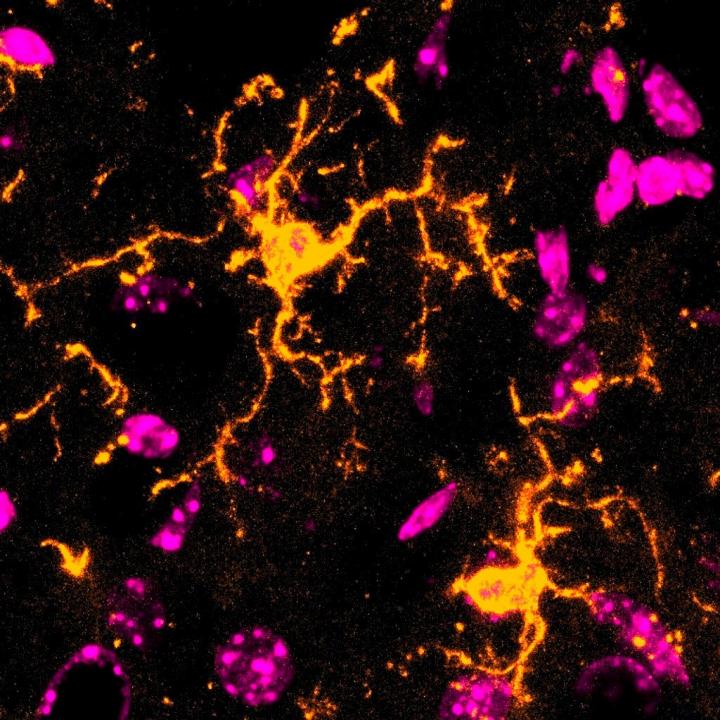
Dr Chopra and his team are focused on studying abnormally fat-rich cells surrounding diseased regions of the brain, including cells called microglia and star-shaped cells called astrocytes.
The association of fat accumulation in the brain with Alzheimer’s is as old as the disease’s initial discovery.
German psychiatrist Alois Alzheimer, after whom the disease has been named, identified abnormalities in the brain of a woman with the disease that now bears his name, including plaques, tangles and cells filled with droplets of fatty compounds called lipids.
However, until recently, these lipid droplets were dismissed as by-products of disease.
But latest discoveries point to a strong link between the neurodegenerative disease and fats in microglia and astrocytes – both cells that support neurons in the brain.
Microscopic images of brain tissue from people with Alzheimer's disease can be seen to have amyloid beta plaques surrounded by microglia.
These microglia cells close to the plaques had an accumulation of fat in such large quantities that they became overloaded and immobilised, the study found.
"Because of these fatty deposits, microglial cells become dysfunctional – they stop clearing amyloid beta and stop doing their job,” Dr Chopra explained.
The extent of accumulation of fat also depended on the patient’s age and disease progression, becoming more prominent as Alzheimer's disease advances, scientists found.
These new findings could establish the foundation for a "new lipid model of neurodegeneration”, Dr Chopra says.
“We think the composition of lipid molecules that accumulate within brain cells is one of the major drivers of neuroinflammation, leading to different pathologies, such as ageing, Alzheimer's disease and other conditions related to inflammatory insults in the brain,” he says.
“The specific composition of these lipid plaques may define particular brain diseases," he says.
Researchers then traced down the pathway to find that abnormally high levels of an enzyme was contributing to the fat accumulation in these brain cells.
"What we've seen is that when we target the fat-making enzyme and either remove or degrade it, we restore the microglia's ability to fight disease and maintain balance in the brain, which is what they're meant to do," Dr Chopra said.
“We reveal a completely new therapeutic angle: Restore microglial metabolism and you may restore the brain's own defence against disease,” said Palak Manchanda, another author of the study.
Scientists reveal role of ‘youth molecule’ in slowing ageing
‘Mileage clock’ found inside brain could help diagnose Alzheimer’s
Plastic from takeaway containers may fuel Alzheimer’s risk, study warns
‘Pioneering’ new weight-loss jab could help keep weight off even after stopping
Scientists find way to develop shark bite-proof suits for divers and surfers
Study claiming weight-loss benefits of apple cider vinegar retracted







