The financial burden of breast cancer on the UK economy is projected to surge by nearly a third, reaching £4.2 billion within the next 25 years, according to new analysis.
The charity Breast Cancer Now has issued a stark warning, stating the UK faces "dire consequences" unless decisive action is taken to ensure "everyone an equal chance of the best diagnosis, treatment and care".
A collaborative study by Breast Cancer Now and the think tank Demos estimates that breast cancer is already costing the UK economy between £3.2 billion and £3.5 billion in 2025.
These figures encompass the direct costs to the NHS for diagnosing and treating the disease, alongside the economic impact of lost productivity when patients or their informal carers are unable to return to work.
The report indicates that without intervention, this total could escalate by 31 per cent to £4.2 billion by 2050.
Claire Rowney, chief executive of Breast Cancer Now, commented on the findings, asserting that the report "sets out loud and clear the huge challenges in tackling breast cancer and the dire consequences we’ll face unless urgent action is taken now to save more lives from the disease and give everyone an equal chance of the best diagnosis, treatment and care".
She added: “Breast cancer is so far from a done deal.
“Our new report exposes the growing scale of the problem and the human and economic prices being paid – with far too many lives tragically being lost to this devastating disease.
“Great strides have been made in tackling breast cancer over past decades, but it still devastates thousands of lives in the UK each day – with people facing long anxious waits for a diagnosis or vital lifesaving treatment, or being denied the life-extending drugs they need.”
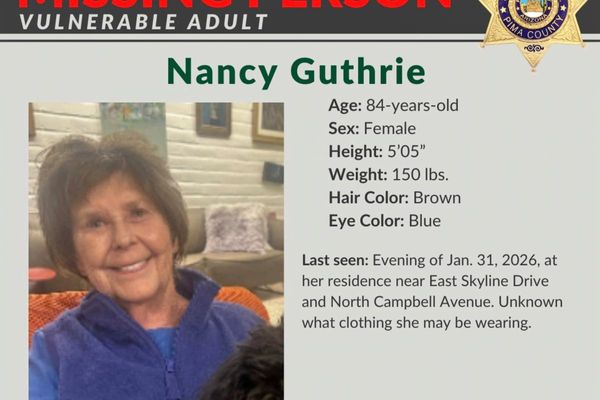
Breast cancer is one of the most common cancers in the UK, with around 56,000 new cases every year and around 11,000 deaths.
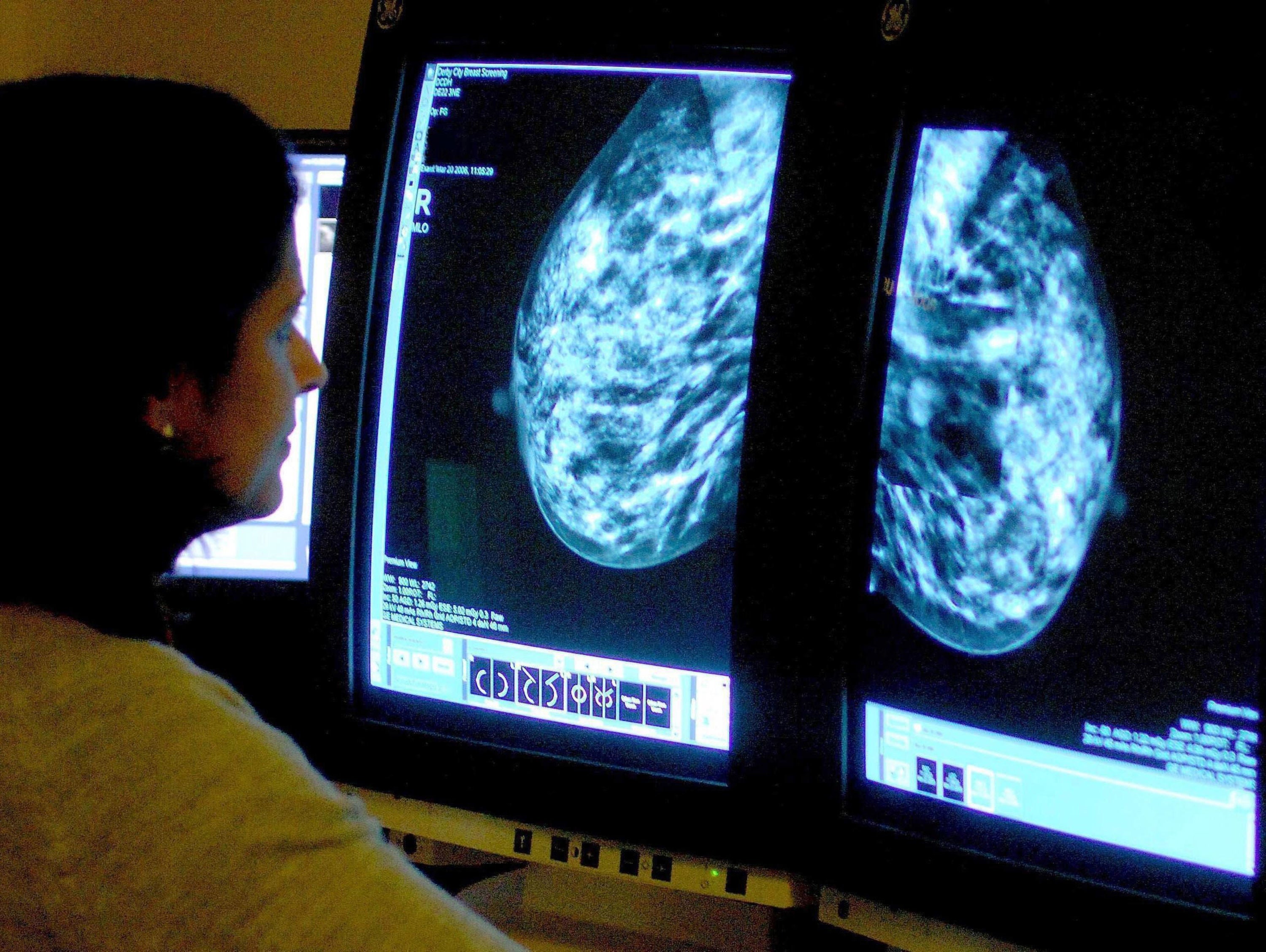
According to the analysis, boosting screening uptake to 80 per cent could generate up to £185 million in savings in 2025 by helping to detect cases earlier and when treatment is more likely to be successful.
Anyone registered with a GP as female will be automatically invited for breast screening every three years between the age of 50 and 71.
Latest statistics show that 70 per cent of women took up their invitation in England in 2023/24, an increase of 5.4 percentage points from the previous year.
Ms Rowney said: “We’re calling on governments and policymakers across the UK to work with Breast Cancer Now and our supporters to urgently implement measures we know will improve the lives of those impacted by breast cancer – including tackling low breast screening uptake rates and reducing health inequalities.
“Measures that will also bring about much-needed cost savings to the NHS and UK economy.”
Danielle Blakesley, 38, from Ilminster, was diagnosed with breast cancer in January 2022 aged 34.
The mother of two had a mastectomy, chemotherapy, radiotherapy and is currently taking tamoxifen to help reduce the risk of the cancer returning, but has been unable to return to work due to the long-term side effects of treatment.
She said: “I’ve been grieving who I once was before my diagnosis, able to be a part of so many things.
“I didn’t realise how intense treatment would be. After the third round of chemotherapy I didn’t want to be here. I didn’t see how my body was going to get through it. I’ve had side effects like nerve damage to my feet and joint pain and issues.
“Even now I struggle when I try to do normal things. Just keeping up with my boys can take its toll. I get short of breath when I try to exercise. I was keen to go back to a job that I loved after treatment, but I haven’t been able to due to my fatigue, joint pain and limited mobility.
“My emotional and mental health has changed dramatically since treatment. I’m trying to live my life but I just have no focus, spark or confidence.”
Meanwhile, the report said taking action to tackle health inequalities could potentially save thousands of lives a year.

The analysis estimates that addressing disparities in breast cancer diagnosis could save 2,000 lives a year in ethnic minority communities and 3,200 lives a year in the most deprived areas, while saving up to £180 million and £389 million respectively for the economy.
Lucy Bush, director of research and participation at Demos, which has been working with Breast Cancer Now since 2023 to model the impact of breast cancer, said: “In the context of the NHS 10 year plan for health announcing a shift ‘from disease cure to disease prevention’ this paper comes at a timely juncture. It helps draw attention to the massive opportunity we have to reduce the impact of this devastating disease on our country.
“Our work sheds a particular light on the difference that could be made by focusing on improving outcomes for ethnic minority and low-income groups.
“The disparity we see in the survival rates between different demographic groups is simply unacceptable and the uplift in wellbeing savings demonstrates what the ultimate prize would be – a reduction in the suffering and early deaths of thousands of people.”