The body mass index (BMI) metric has caused "historical harm," including racist exclusion, according to a new report by the American Medical Association (AMA) Council on Science and Public Health.
Why it matters: Doctors have long relied on BMI to measure obesity, but it is an imperfect measurement that does not directly assess body fat, the nation's largest medical association said this week.
Driving the news: BMI is measured by dividing a person's weight in kilograms or pounds by the square of height in meters or feet.
- Cutoffs for BMI, which range from underweight to obese, were created based on data collected from non-Hispanic white populations and do not take into account gender or ethnicity, according to the report.
- Body fat "does not account for differences across race/ethnic groups, sexes, genders, and age-span," the AMA said.
Be smart: At the same BMI, women tend to have more body fat than men, and older people have more body fat than younger adults, per the CDC.
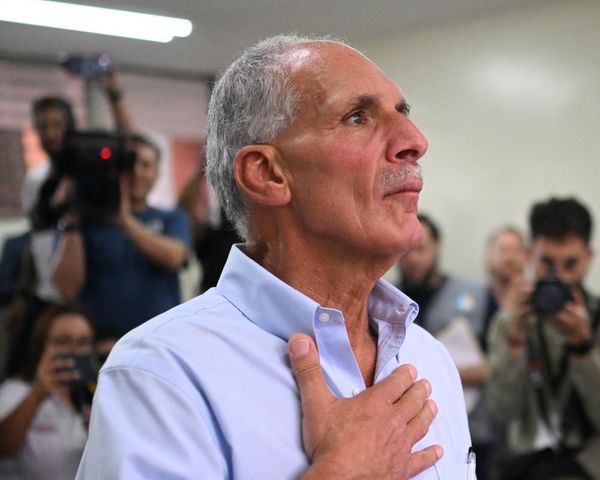
What they're saying: “It is important for physicians to understand the benefits and limitations of using BMI in clinical settings to determine the best care for their patients," Dr. Jack Resneck, Jr., the AMA's immediate past president, said in a statement.
- "Relative body shape and composition heterogeneity across race and ethnic groups, sexes, genders and age-span is essential to consider when applying BMI as a measure of adiposity," the AMA said.
Between the lines: BMI does not account for the full range of eating disorders and is problematic when used to treat them, according to the report.
- The metric can contribute to stigma around weight and be a barrier in accessing care for people with eating disorders, said Lauren Smolar, a spokeswoman for the National Eating Disorders Association.
- "Eating disorders occur to people at higher weights but are diagnosed at a much lower rate, because health providers do not look into additional health concerns beyond body size," she said.
What's next: Moving forward, physicians should be educated on the issues with BMI and alternative measures to diagnose obesity, the report said.
- The new policy suggests that BMI could be used in conjunction with a host of other measures in clinical settings, such as: visceral fat; body adiposity index; body composition; relative fat mass; waist circumference; and genetic or metabolic factors.