New brain scans from people with psychosis may confirm a long-standing theory as to why people experience these sudden breaks from reality.
The theory states that, in psychosis, brain networks in charge of directing a person's attention malfunction. This causes a person to experience hallucinations, or sensations of things that aren't actually happening; and delusions, or unshakable false beliefs. Psychosis is a feature of serious mental disorders such as schizophrenia, but its symptoms exist on a continuum and can also occur independently of any defined mental disorder.
The precise details of what happens in the brain to cause psychosis have long eluded scientists. One reason for this is that psychosis is often studied in people who have long been taking antipsychotic medications, so it's difficult to distinguish brain changes tied to the condition from those linked to the drugs.
A goal of the new brain-scan study, published April 11 in the journal Molecular Psychiatry, was to pinpoint the underlying mechanisms involved in psychosis from an early age, which could help pave the way to earlier diagnoses and better treatments.
Related: A mysterious brain network may underlie many psychiatric disorders
"The abnormalities do not start when you are in your 20s; they are evident even when you are 7 or 8," lead study author Kaustubh Supekar, a clinical associate professor of psychiatry and behavioral sciences at Stanford University School of Medicine, said in a statement.
To spot these abnormalities, the study focused on people ages 6 to 39 with a rare genetic condition associated with psychosis, called 22q11.2 deletion syndrome. People with the syndrome are missing part of one of their copies of chromosome 22. In addition to having a risk of other conditions — such as heart abnormalities, attention-deficit/hyperactivity disorder (ADHD) and autism — those affected with the syndrome have a roughly 30% chance of experiencing psychosis, schizophrenia or both.
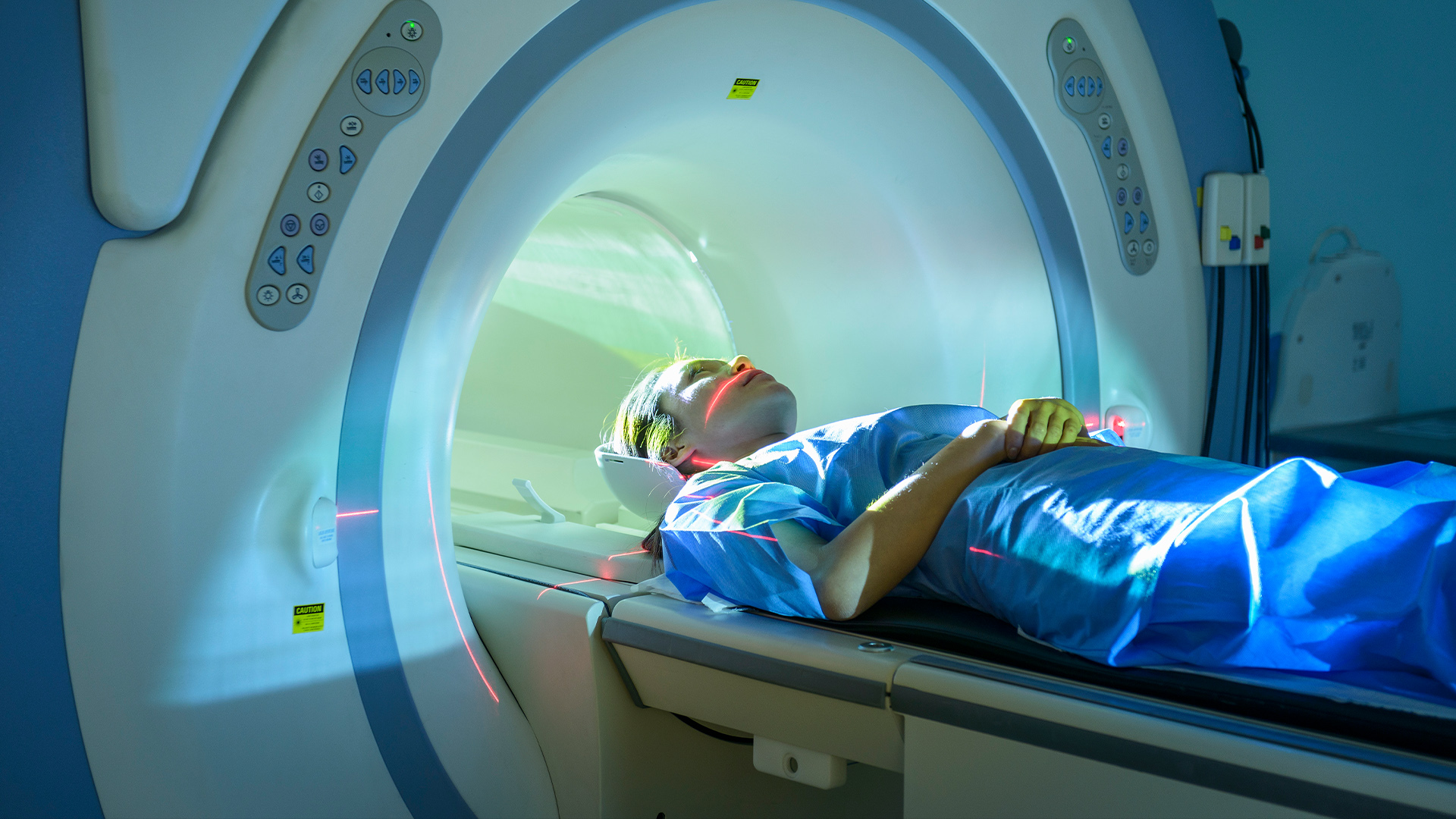
The team collected brain data using functional magnetic resonance imaging (fMRI), which tracks changes in blood flow that correspond with brain cell activity. There were nearly 900 people involved, including 101 people with 22q11.2 deletion syndrome, some with psychosis and some without, and 120 with "psychosis of unknown origin."
In addition, the study included people with no history of psychosis for comparison, as well as people with ADHD and autism, "which classification studies rarely do," said Dr. Rick Adams, a fellow in mental health neuroscience at the University College London who was not involved in the study. This was "a big plus" because it helped show that the brain signatures they found are specific to psychosis and not seen in other brain-related disorders, Adams told Live Science in an email.
With help from colleagues in computer science at Stanford, the team created a new machine learning algorithm to uncover patterns in the fMRI data. The tool revealed overlapping "signatures" in the brains of people with 22q11.2 deletion syndrome and associated psychosis or with psychosis of unknown causes.
These signatures, which did not appear in any of the comparison groups without psychosis, showed up in two key components of what's known as the brain's "salience network." This network's job is to dynamically switch our attention between internal thoughts and external stimuli, essentially directing our attention to what's important and real. The brain scans show that two nodes in this network are most crucial to psychosis: the anterior insula, which works to filter out unimportant information; and the ventral striatum, which predicts which information will be most rewarding or important to us.
These results "fit with prior hypotheses about the disorder," Adams said. They build upon theories about the salience network and psychosis that were based on the brain's structure, rather than its function, as well as more recent work that started to look at its function. The study also backs up work done in earlier studies that investigated the brain mechanisms behind psychosis in 22q11.2 deletion syndrome, specifically.
The researchers now plan to target these two key brain areas with existing treatments, such as brain stimulation, to see if they can prevent or delay psychosis in people at high risk of the condition. They also plan to study how antipsychotic medications affect these parts of the salience network, to reveal exactly how they work.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line "Health Desk Q," and you may see your question answered on the website!