Nearly 40 percent of terminal cancer patients suffered physical pain in the month before passing, according to results of the first national survey investigating this issue revealed at the end of December last year. Today, when one in three Japanese die from cancer, the question of whether the pain of cancer can be controlled is an immediate and important one. We looked into the issue at the sites where terminal care is provided.
Surveying the bereaved
A woman in Nagoya in her early 80s who had been diagnosed with the most advanced stage 4 breast cancer decided of her own volition not to be treated, but continued to have her progress observed as an outpatient at Fujita Health University Hospital in Toyoake, Aichi Prefecture. In November last year, she suffered severe back pain due to metastasis while in a short-stay facility. A visiting doctor prescribed painkillers, but they had no effect, and the pain gradually worsened.
The woman was then admitted to the palliative care center at the clinic, where she took a prescribed medical narcotic at a dosage of two tablets per day, and her pain completely disappeared two days later.
She regained her appetite and was able to join conversations with other patients over a cup of tea at the clinic. She was pleased, saying that "the pain went away and my mood has become brighter."
The nationwide survey was conducted by the National Cancer Center Japan. With the aim of gaining an understanding of the actual conditions of medical treatment in the final stages of human life, about 4,800 bereaved families of patients who had died from cancer or other diseases in 2016 were surveyed during February and March last year through a mailed questionnaire.
Regarding cancer, 1,630 people or 51 percent of 3,204 people surveyed provided valid responses. When asked whether the patient "was able to spend the last month of life in less pain," 36 percent of respondents suggested that the patient was suffering pain by choosing such answers as "disagree" and "somewhat disagree."
Meanwhile, when asked whether medical professionals responded promptly to the pain, as many as 84 percent answered that they did respond, with answers such as "agree" and "somewhat agree." These results suggest that there are a considerable number of cases where "the doctor responded promptly but was not able to relieve the pain caused by the cancer."
This survey does not go so far as to gain a sense of the quality of the medical care, in terms of whether the pain is one that cannot be relieved no matter what kind of medical treatment, or whether the treatment was inappropriate, according to Masashi Kato, the chief of the Division of Medical Support and Partnership at the center.
Nevertheless, Kato went on to explain that "Measures to deal with such pain have to be considered because the results revealed that nearly 40 percent of cancer patients suffer pain."
At the end of January, the center was to commence a full-scale survey targeting about 50,000 people.
Emphasis on palliative care
In 2008, the Health, Labor and Welfare Ministry started a palliative care (see below) workshop for doctors working at designated cancer hospitals and other medical institutions. The workshop already has more than 100,000 participants. Last year, it expanded its participants beyond doctors to include nurses and other medical professionals. It also frequently revises fees for medical treatment so that medical institutions that provide good palliative care can enjoy increased income.
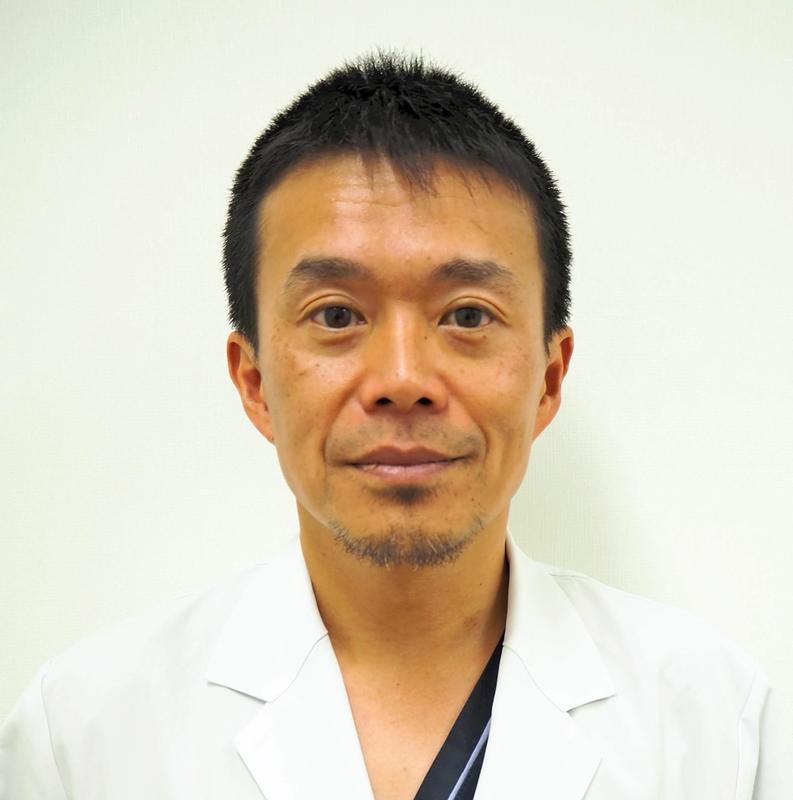
"Palliative care in the nation has improved considerably compared to 10 years ago. However, there are still differences in the level of care, depending on the locality, hospital and doctor," said Prof. Takashi Higashiguchi, the director of the palliative care center at Fujita Health University Hospital.
The woman with breast cancer described at the beginning of this story was prescribed analgesics by a doctor at the short-stay facility, but it was paracetamol, which is commonly prescribed for symptoms such as everyday headaches and menstrual cramps.
Higashiguchi said not a few doctors still hesitate to use medical narcotics. Behind a lack of knowledge in palliative care are medical practices, including refraining from using medical narcotics until patients suffer severe pain and using an insufficient amount of narcotics.
"Pain caused by cancer can be virtually eliminated if appropriate treatment is carried out," said Higashiguchi. "Doctors should not hesitate to use medical narcotics at an early stage so patients will not suffer pain regardless of regions or medical institutions."
People unnecessarily endure suffering
Dr. Ryo Yamamoto, head of the palliative internal medicine department of the Saku Central Hospital Advanced Care Center and director of the Japanese Society for Palliative Medicine, answered questions about cancer pain.
-- Do all cancer patients suffer from pain?
About half the patients being treated for cancer feel pain, with the rate going up to two-thirds in cases of progressive cancer. There are also patients who suffer no pain even though they have progressive cancer.
-- What causes the pain?
It depends whether the cancer is in areas that are sensitive to pain. For example, pancreatic cancer tends to cause pain due to the spot where many nerves congregate in the back of the pancreas. On the other hand, lung cancer usually brings little pain because the lung has fewer parts that are sensitive to pain. However, if cancer is found outside of the lungs, it may cause pain since the chest lining around the lungs is sensitive to pain.
-- Is there any established procedure for treating cancer pain?
Treatments of cancer pain are based on World Health Organization guidelines. Common painkillers are used if the pain is mild, while narcotics, or opioid analgesics such as morphine and oxycodone, are prescribed for stronger pain.
-- Do narcotics like morphine passively hasten patients' death, or result in addiction?
Numerous studies have found that narcotics do not shorten a person's lifespan. When healthy people use them, they can become addicted. However, addiction is not likely in the case of terminal cancer patients. There is no limit on dosage, and patients can take as much as needed to ease their pain.
-- Some people believe it's better for the health not to take any medicine if the pain is bearable.
Pain increases when no measures are taken. Japanese people tend to think endurance is a virtue, but there is no point to enduring cancer pain. I hope more and more patients tell their doctors about their pain. If there are no doctors specialized in palliative care at your local hospitals, you can seek support from the nearest cancer consultation center at designated cancer hospitals.
(From The Yomiuri Shimbun, Jan. 30, 2019)
-- Palliative care
Medical treatment and care that lessen physical and mental suffering caused by pain, and relieve the anxieties involved in a life in society for patients suffering life-threatening diseases such as cancer, together with their family members. Palliative care is not limited to the terminal stage, but can be provided in parallel with treatment from an early stage.
Read more from The Japan News at https://japannews.yomiuri.co.jp/