With the year 2025 approaching, when all baby boomers will turn 75 or older, the details of changes in medical treatment fees for fiscal 2018 have been finalized. The revision of medical treatment fees is being done simultaneously with the revision of nursing care fees -- the first time they have coincided in six years. With the goal of enabling the elderly to spend their final days in their familiar local communities, the revision of medical treatment fees for fiscal 2018 focused on promoting collaboration between medical and nursing care and enriching home-based medical treatment.
In early January, a 69-year-old man living in Sumida Ward, Tokyo, sounded upbeat for the first time in quite a while.
"The pain is gone, and I was able to get a good night's sleep," he said.
The medical narcotic he had taken had been effective.
Ko Kawagoe, 70, director of Clinic Kawagoe in Sumida Ward, which centers on regular visits to patients in home-based treatment, told him, "Don't just put up with the pain; let me know about it."
In autumn last year, it was found that the man's kidney cancer had spread to his hip bone. He initially unhappily endured the strong pain daily, but Kawagoe and his nursing staff visited his house every day at the end of last year and in early January this year.
His care manager also received information from the nursing staff and visited his home many times to determine whether any nursing care services were required. Due to the attentive care he received, he said, "I feel much better after the treatment."
As cancer patients approach the last moments of their lives, they quickly lose the ability to perform daily tasks such as making meals and changing clothes by themselves. If proper care is not given, hospitalization is sometimes required.
"It's important that care is provided in accordance with the conditions of each patient so that they can spend their last days with peace of mind," Kawagoe said.
'High-death society'
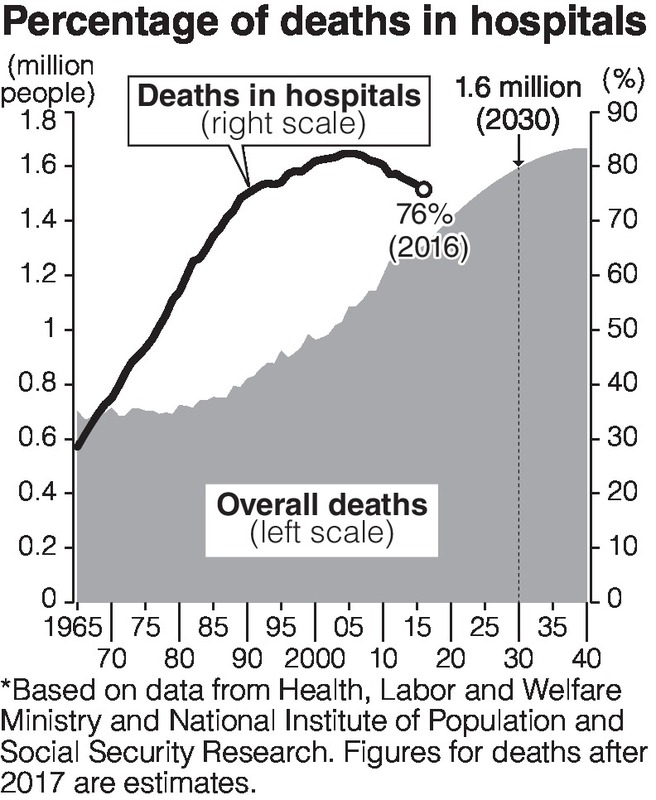
With the continued aging of Japan's population, the Health, Labor and Welfare Ministry estimates that by the year 2025, there will be about 1 million people receiving at-home medical care services, or about 1.5 times more than the 2014 figure of about 650,000. The number of deaths per year will reach about 1.6 million by 2030, heralding the arrival of a so-called "high-death society."
Currently, more than 70 percent of all deaths occur in hospitals, but it is expected that hospitals alone will not be able to support this proportion in the future.
Therefore, the simultaneous revisions of medical treatment fees and nursing care fees placed emphasis on promoting home-based treatment and a system in which patients are attended to at home during their final days by strengthening cooperation between medical and nursing care treatment.
One such effort to enhance the collaboration is between doctors who visit the homes of patients and the managers of nursing care services.
For patients with terminal cancer who receive treatment at home, the medical treatment fee system will require doctors, when they receive a monthly management fee of up to 54,000, yen to share information with care managers and enable the provision of necessary nursing care services in the event of a sudden change in a patient's condition.
On the other hand, the nursing care fee system will enable care managers, who periodically visit patients' homes to understand their conditions and share this information with doctors, to receive up to 4,000 yen per month.
Special facilities
The government will also support patients at nursing care facilities who are attended to by families or others in their final days.
Special nursing care facilities for the elderly are expected to play the role of "end-of-life residences." However, according to a fiscal 2016 survey by the Health, Labor and Welfare Ministry, 16 percent of respondents of such special nursing care facilities said they would transfer patients nearing the end to a hospital or similar facility. One of the main reasons for this is that, although the majority of special nursing care facilities have part-time doctors who are available as needed, it is a significant burden on such a part-time doctor to work round-the clock.
The fee revisions this time allowed high medical fees for doctors who are not part-time when they visited special nursing care facilities to provide care to patients in their final days. In addition, the nursing care fee revision will establish a system in which part-time doctors who are called on to provide care late at night or early in the morning can receive remuneration.
"These simultaneous revisions will increase the number of cases in which patients are attended to in their final days outside hospitals," said Mitsunori Nishikawa, director of the regional medical cooperation office at the National Hospital for Geriatric Medicine in Obu, Aichi Prefecture. "We hope medical and nursing care staff will cooperate to realize the wishes of patients that medical and nursing staff have come to know through long-term exchanges with the patients."
Deep-rooted trust in major hospitals behind special fee
By Kazuki Nishihara / Yomiuri Shimbun Staff Writer
In anticipation of an increasing number of dementia patients and patients with lifestyle-related diseases who need daily health management, the government aims for a shift in emphasis from hospital-based medical treatment to that based on a "regular family doctor."
First, 800 yen will be added to the initial examination by a doctor who can be reached 24 hours a day, increasing the function of family doctors.
The number of dementia patients is expected to climb from about 4.6 million in 2012 to about 7 million in 2025.
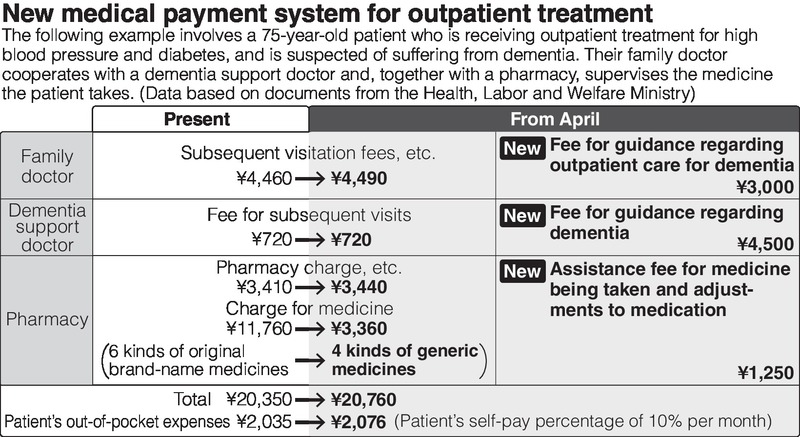
To provide appropriate treatment, when a family doctor is advised by a "doctor certified by the government to support dementia patients," both doctors will receive remuneration.
Cooperation with pharmacies will also be promoted to reduce the overmedication of patients who are taking multiple drugs.
The Health, Labor and Welfare Ministry released preliminary calculations showing that, even if family doctors had their remuneration increased in cooperation with dementia-support doctors, the burden on patients could be kept from greatly increasing by reducing overmedication and switching to cheaper generic drugs.
However, patients have strong trust in major hospitals. Therefore, the revision this time will increase the number of hospitals that are allowed to collect a special fee of 5,000 yen or more when a patient consults a doctor at a major hospital without a referral.
For cases requiring acute care to deal with surgery and serious illnesses, the "seven-to-one" proportion system, in which one nurse is responsible for seven such patients under careful treatment, has become impractical. The system charges a patient the highest basic fees for hospitalization.
Along with requiring a higher proportion of serious patients, the revision aims to make a switch to a remuneration system based on actual medical care performances.
"I think the revision this time will lead to a reorganization of acute-care facilities in accordance with regional needs," said Shunya Ikeda, a professor of medical economics at the International University of Health and Welfare. "Going forward, it will be essential to introduce performance metrics to value high-performing hospitals and further improve the quality of the medical treatment they provide."
Another issue is how to promote the efficiency of medical care as a whole.
Some advocate the idea of expanding the number of hospitals requiring patients to pay a special fee for receiving care at major hospitals without referrals.
In the revision of drug prices, a full-scale introduction of cost-effectiveness assessment was postponed to fiscal 2019 or beyond.
With an increase in medical expenses due to the aging society, bold steps toward reform will be necessary.
(From The Yomiuri Shimbun, Feb. 8, 2018)
Read more from The Japan News at https://japannews.yomiuri.co.jp/







